Session Information
Date: Tuesday, November 9, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III (1836–1861)
Session Type: Poster Session D
Session Time: 8:30AM-10:30AM
Background/Purpose: Gastrointestinal dysfunction (SSc-GI) is a significant burden to patients with systemic sclerosis (SSc), particularly in those with longstanding disease. The management of SSc-GI is often challenging. Whilst hallmark mechanisms including vasculopathy, fibrosis, and inflammation underlie gut pathogenesis, reflected in autoantibody (ANA) associations, off-target effects of drugs used in SSc may contribute to GI dysfunction. We sought to discover and confirm associations with SSc-GI dysfunction in a Phenome-Wide Association Study (PheWAS).
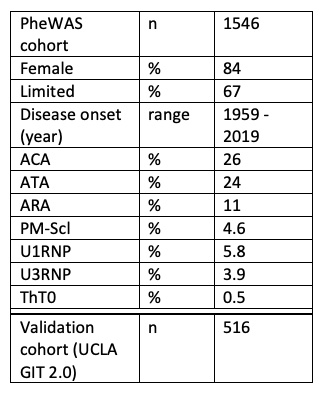
Methods: Archived clinic letters (12,535 letters) of 2,058 consented patients at the Royal Free Hospital (UK) between 2002-2021 were parsed into a database. Patients with at least three letters were included. Two ‘dictionaries’, one of diagnoses (Disease Ontology project CC0, modified to included ANA) and another of drugs (DrugBank Open Data CC0) were used to label each patient. Using the PheWAS approach for six SSc-GI outcomes (constipation, diarrhoea, dysmotility, incontinence, reflux, small intestinal bacterial overgrowth [SIBO]), we assessed every diagnosis and drug in univariate logistic regressions. P values were adjusted for false discovery rate (Benjamini-Hochberg). Significant PheWAS predictors (p < 0.05) were validated against the UCLA GIT 2.0 questionnaire score (UCLA GIT) in a second dataset of 516 patients including total GI, reflux, bloating, diarrhoea, soilage, constipation, social, and emotional scores.
Results: Table 1 presents cohort demographics. Using the diagnosis and drug dictionaries, we identified 673 diagnoses (including ANAs) and 634 drugs. Top drugs (prevalence): omeprazole 56%, losartan 49%, lansoprazole 42%, and mycophenolate mofetil (MMF) 40%; top diagnoses: limited SSc 65%, Raynaud’s 50%, interstitial lung disease (ILD) 36%, and overlap 27%.
PheWAS analysis demonstrated significant associations across the six key SSc-GI outcomes (Fig. 1). Constipation was linked to fentanyl (OR = 12), amitriptyline (OR = 3.3), migraine (OR = 14), ANA negative (OR = 4.8), aspiration (OR = 15), and incontinence (OR = 5.3). Diarrhoea was linked to ambrisentan (OR = 9.5) and ACA (OR = 3). Dysmotility was linked to ANA homogenous (OR = 6.3), tamsulosin (OR = 6.9), fentanyl (OR = 6.1), and oxycodone (OR = 12). Incontinence was linked to ACA (OR = 3.9), ambrisentan (OR = 8.6), and inversely linked to MMF (OR = 0.27). Reflux was linked to ILD (OR = 1.7) and ANA homogenous (OR = 7.7). SIBO was linked to ACA (OR = 2.5), total parenteral nutrition (OR = 11), osteoporosis (OR = 2.9), and anemia (OR = 2.9).
Significant PheWAS associations were validated against UCLA GIT domain scores (Fig. 2). For the total GI score – 18 drugs and 3 diagnoses were validated; soilage – 6 drugs, 1 ANA, and 2 diagnoses; reflux – 17 drugs and 2 diagnoses; bloating – 11 drugs and 2 diagnoses; diarrhoea – 7 drugs; social – 19 drugs and 3 diagnoses; emotional – 17 drugs and 5 diagnoses; constipation – 2 ANA, 9 drugs, and 2 diagnoses.
Conclusion: Using a hypothesis-free PheWAS approach, we revealed potential contributors to SSc-GI dysfunction, including drugs such as opioids, anti-muscarinics, and endothelin receptor antagonists; and ANAs including ACA, ANA-homogenous and ANA-negative subtypes.
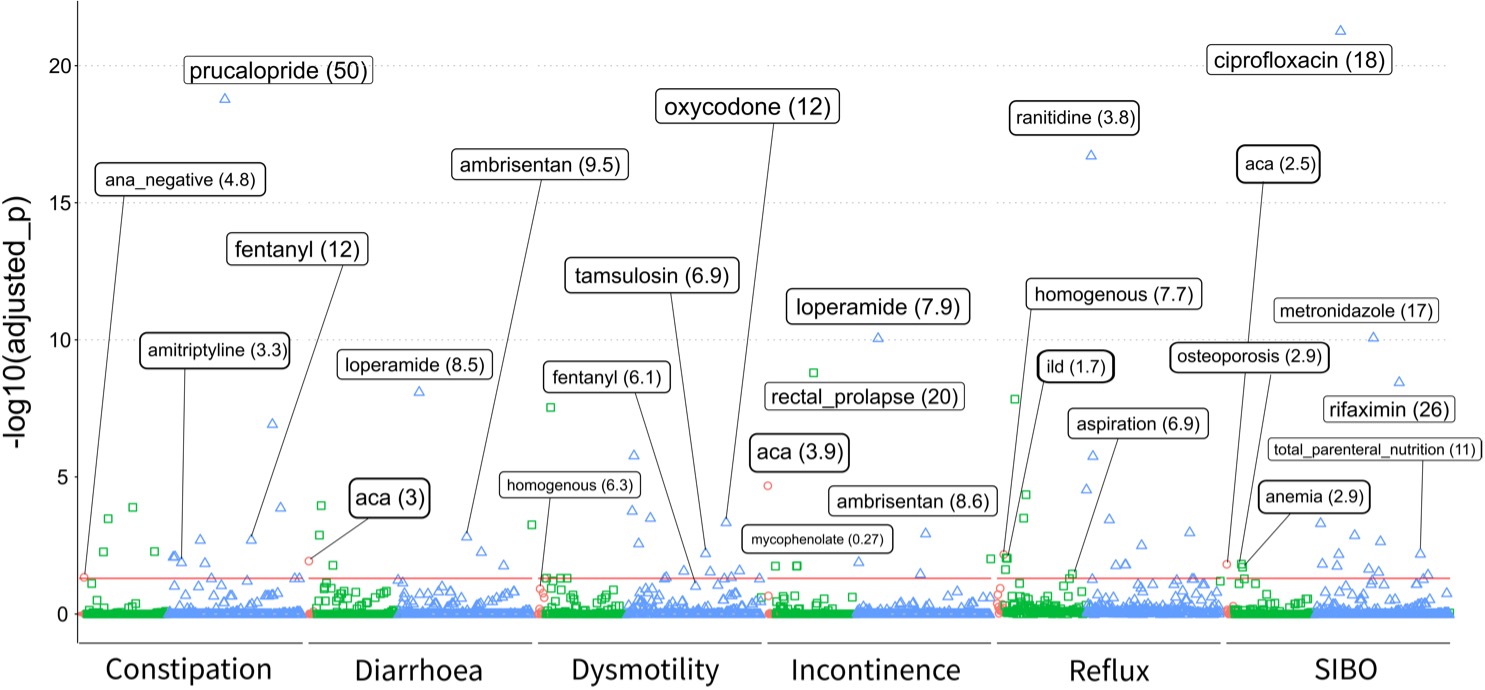 Figure 1. PheWAS analysis demonstrated significant associations between ANAs (red circles), diagnoses (green squares), and drugs (blue triangles) in six key SSc-GI areas. The red horizontal line indicates adjusted p values < 0.05. Key associations with named variables are presented; odds ratios in brackets.
Figure 1. PheWAS analysis demonstrated significant associations between ANAs (red circles), diagnoses (green squares), and drugs (blue triangles) in six key SSc-GI areas. The red horizontal line indicates adjusted p values < 0.05. Key associations with named variables are presented; odds ratios in brackets.
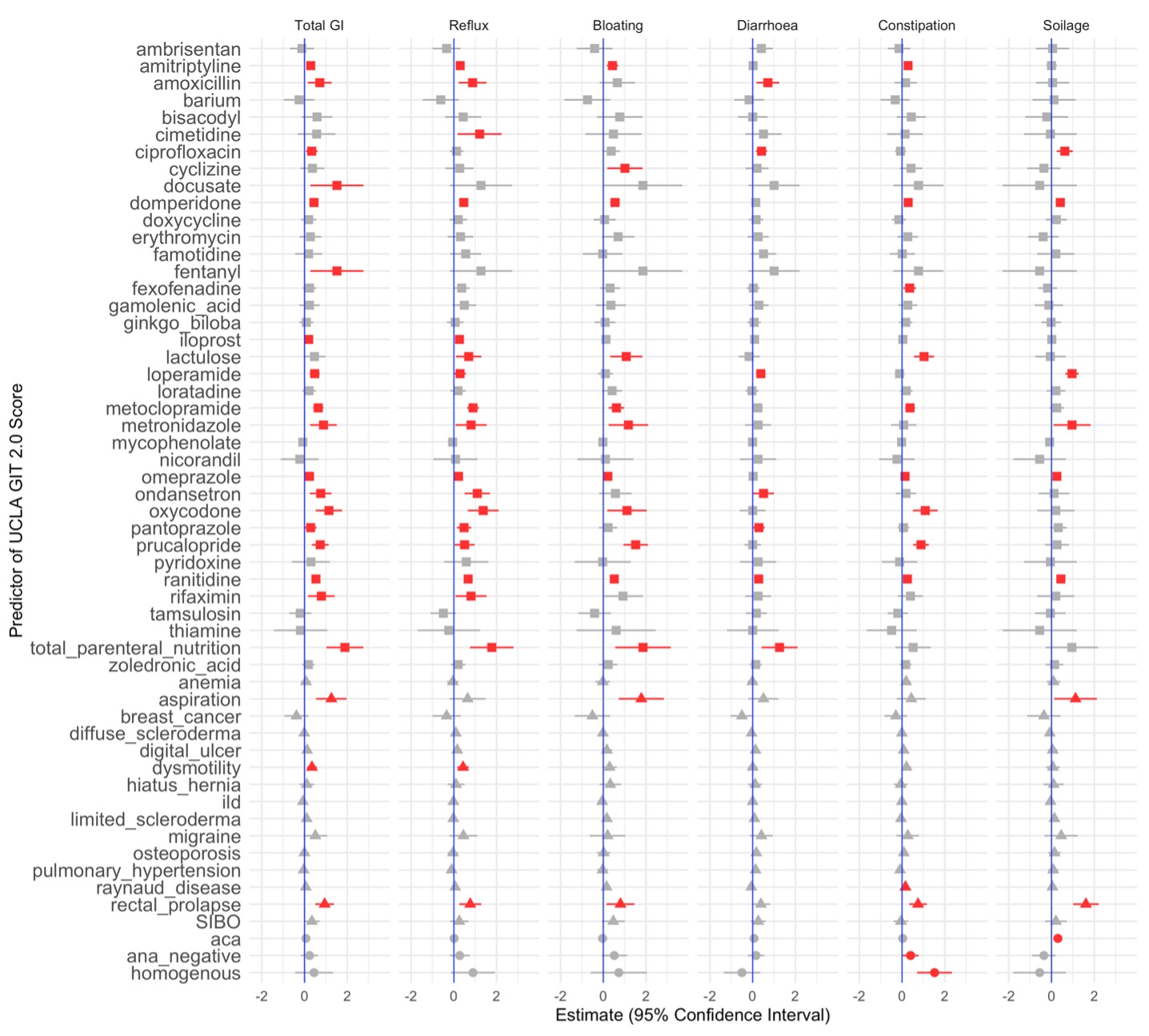 Figure 2. PheWAS hits were validated in a linear model against UCLA GIT 2.0 domain scores: total GI, reflux, bloating, diarrhoea, constipation, and soilage domains are shown. Estimates with 95% CIs are presented; red highlights p < 0.05. Square – drugs; triangle – diagnoses; circle – ANA.
Figure 2. PheWAS hits were validated in a linear model against UCLA GIT 2.0 domain scores: total GI, reflux, bloating, diarrhoea, constipation, and soilage domains are shown. Estimates with 95% CIs are presented; red highlights p < 0.05. Square – drugs; triangle – diagnoses; circle – ANA.
To cite this abstract in AMA style:
Maclean R, Ahmed F, Ong V, Murray C, Denton C. Untangling the Gut: A Phenome-Wide Association Study of Drugs and Diseases with Gastrointestinal Dysfunction in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/untangling-the-gut-a-phenome-wide-association-study-of-drugs-and-diseases-with-gastrointestinal-dysfunction-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/untangling-the-gut-a-phenome-wide-association-study-of-drugs-and-diseases-with-gastrointestinal-dysfunction-in-systemic-sclerosis/