Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Primary Sjögren’s syndrome (pSS) is an autoimmune disease characterised by glandular involvement of the eye and salivary glands, leading to xerostomia and xerophthalmia. In addition, this involvement can damage other organs such as the lung, kidney, central and peripheral nervous system. Sustained inflammatory activity can lead to non-Hodgkin’s lymphoma. At present, our knowledge of the molecular alterations underlying different clinical phenotypes is still limited.
We aim to characterise the circulating inflammatory profile of pSS patients, using next-generation proteomic studies, in order to identify new biomarkers and distinctive clinical subgroups.
Methods: In an 89 SSp patients cohort from a multicentre study between Ospedale Maggiore Policlinico in Milan and Hospital Reina Sofia in Cordoba, a 92 inflammation-related serum proteins panel was analysed using the innovative Proximity Extension Assay (PEA, Olink) technology. In parallel, a comprehensive clinical profile was performed, including measures of activity (ESSDAI), cumulative damage (SSDDI), patient-reported damage (ESSPRI), health-related quality of life (HRQoL) questionnaires for general health (SF-36), patient-reported damage (ESSPRI), as well as main clinical complications and the prevalence of circulating autoantibodies.
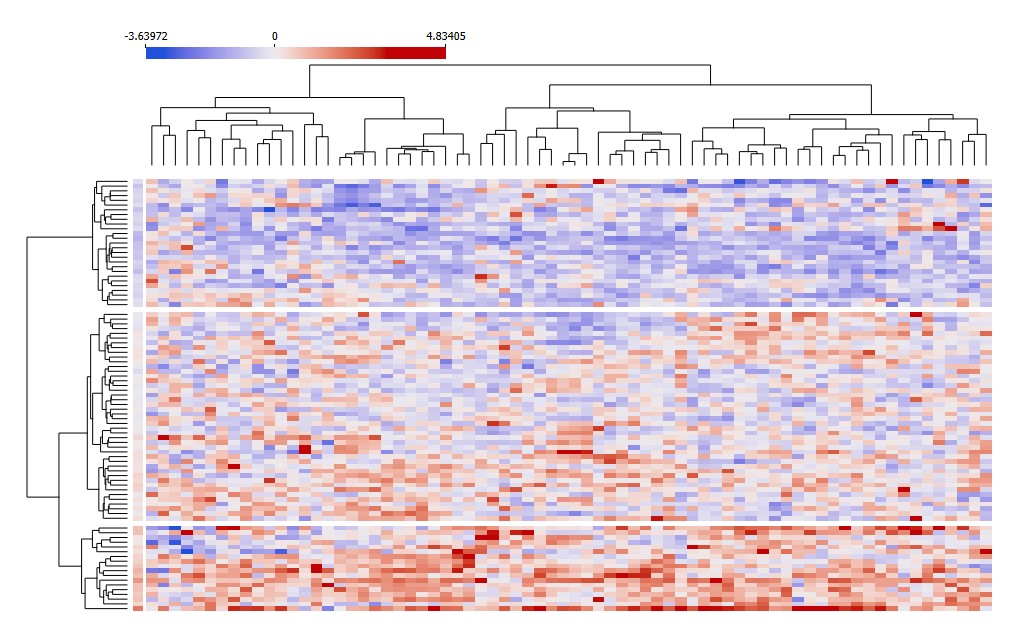
Unsupervised clustering analysis (ward’s method) was applied to identify subgroups of patients based on their proteomic profile; associations with clinical and laboratory variables were performed by means of ANOVA and Fisher’s test.
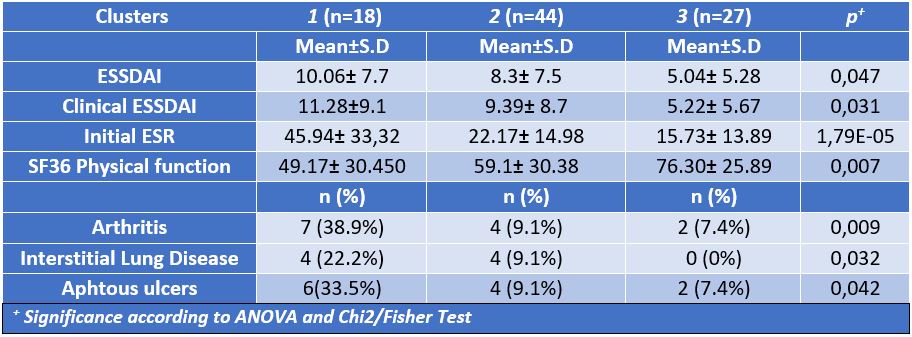
Results: Unsupervised clustering analysis in pSS patients distinguished three groups based on their inflammatory profile. Clusters 1 and 3 had a well characterized proteomic profile (high and low expression, respectively) Further analyses showed that the biological profile well mirrored clinical characteristics: Cluster 1, the most inflammatory, showed higher prevalence of interstitial lung disease, arthritis and aphthous ulcers, higher ESSDAI activity index and lower SF36 physical function score; cluster 3, had the lowest prevalence of symptoms.
43 differentially expressed proteins were identified among clusters. Cluster 1 highlighted chemokines (MCP-1, CXCL11, CXCL9, CCL4, SLAMF1, MCP-4, CCL11, CCL19, CCL3, CXCL10, X4E-BP1, IGN-gamma, MCP-2, CASP-8, CCL20), growth factors (VEGF-A, TGFb-1, TGF-α, FGF-23, GFG-21, HGF, CSF-1), interleukins (IL8, IL6, IL17C, IL18, IL10Ra, IL10Rb, IL18R1, IL12b, TNFSF14, TNF, TNFRSF9, TNFB), membrane proteins (CD8A, CDCP1, OPG, PDL1, CD5,
CD40) and enzymes (uPA, MMP1, ADA). These alterations could be associated with an increased invasive capacity of immune cells. Furthermore, these proteins levels correlated with clinical ESSDAI, highlighting their potential as biomarkers of disease activity.
Conclusion: The analysis of the circulating inflammatory profile of pSS patients, using new high-throughput proteomic technologies, allows the identification of distinctive molecular signatures associated with relevant clinical profiles. Identifying novel biomarkers of activity has the potential to significantly enhance the precision and personalization of disease monitoring for this condition.
To cite this abstract in AMA style:
Sequí-Sabater J, Perez-Sanchez C, Meoni C, Cerdó-Ráez T, Abalos-Aguilera M, Ruiz Vilchez D, Cepas F, Barbarroja N, Escudero A, Aguirre M, Lopez-Pedrera C, Beretta L. The Inflammatory Proteome in Sjögren’s Syndrome Identifies New Biomarkers and Relevant Clinical Subgroups [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-inflammatory-proteome-in-sjogrens-syndrome-identifies-new-biomarkers-and-relevant-clinical-subgroups/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-inflammatory-proteome-in-sjogrens-syndrome-identifies-new-biomarkers-and-relevant-clinical-subgroups/