Session Information
Date: Tuesday, October 28, 2025
Title: Abstracts: Systemic Lupus Erythematosus – Animal Models (1758–1763)
Session Type: Abstract Session
Session Time: 10:30AM-10:45AM
Background/Purpose: Approximately 90% of patients with systemic lupus erythematosus are women, and skin is one of the most frequently affected organs. We previously found that the transcription coregulator VGLL3 is enriched in the keratinocytes of healthy women, where it promotes expression of inflammatory genes. We subsequently showed that mice with epidermal overexpression of VGLL3 develop cutaneous and systemic lupus-like autoimmune disease. However, the value of VGLL3 as a therapeutic target in lupus remains unknown.
Methods: We have combined mouse modeling and investigations in human skin to explore VGLL3 as a potential therapeutic target in lupus. To gain insight into VGLL3-related disease mechanisms, we developed several novel transgenic mouse models that enable us to reverse epidermal VGLL3 overexpression, test VGLL3 necessity for cofactor binding, and robustly induce VGLL3 in adulthood. Furthermore, we used in vitro IP-mass spectrometry (IP-MS) as well as proximity ligation assay to identify VGLL3 binding partners in human keratinocytes and skin from discoid lupus erythematosus (DLE) patients, respectively.
Results: We determined that normalization of epidermal VGLL3 activity ameliorates skin and select systemic manifestations of VGLL3-induced murine lupus. Through in vitro IP-MS, we identified TEAD1 and TEAD3 as major binding partners of VGLL3 in human keratinocytes, while our proximity ligation assay data showed nuclear colocalization of VGLL3 and TEAD transcription factors in the epidermis of healthy human individuals and in patients with DLE, with increased detection in the latter. Exploiting our novel transgenic mouse models, we determined that TEAD binding capacity is required for epidermal VGLL3 to cause murine lupus-like disease. Mutations in the binding site where VGLL3 interacts with TEADs abrogated disease development in mice that overexpress VGLL3 in the epidermis. Furthermore, induction of epidermal VGLL3 overexpression in adulthood resulted in rapid onset of murine lupus that was attenuated by simultaneous epidermal deletion of Tead1, resulting in significantly improved survival. Similarly, pharmacologic inhibition of VGLL3-TEAD binding improved survival of mice with epidermal VGLL3 overexpression. Currently, we are testing additional drugs that are predicted to target TEAD interaction with transcription coregulators for therapeutic effect utilizing both our innovative lupus mouse models and human patient skin explants.
Conclusion: The results of this work show the relevance of VGLL3-TEAD interaction in murine lupus-like disease development and are anticipated to provide vital preclinical data supporting the approach of VGLL3-TEAD inhibition in lupus patients with skin involvement.
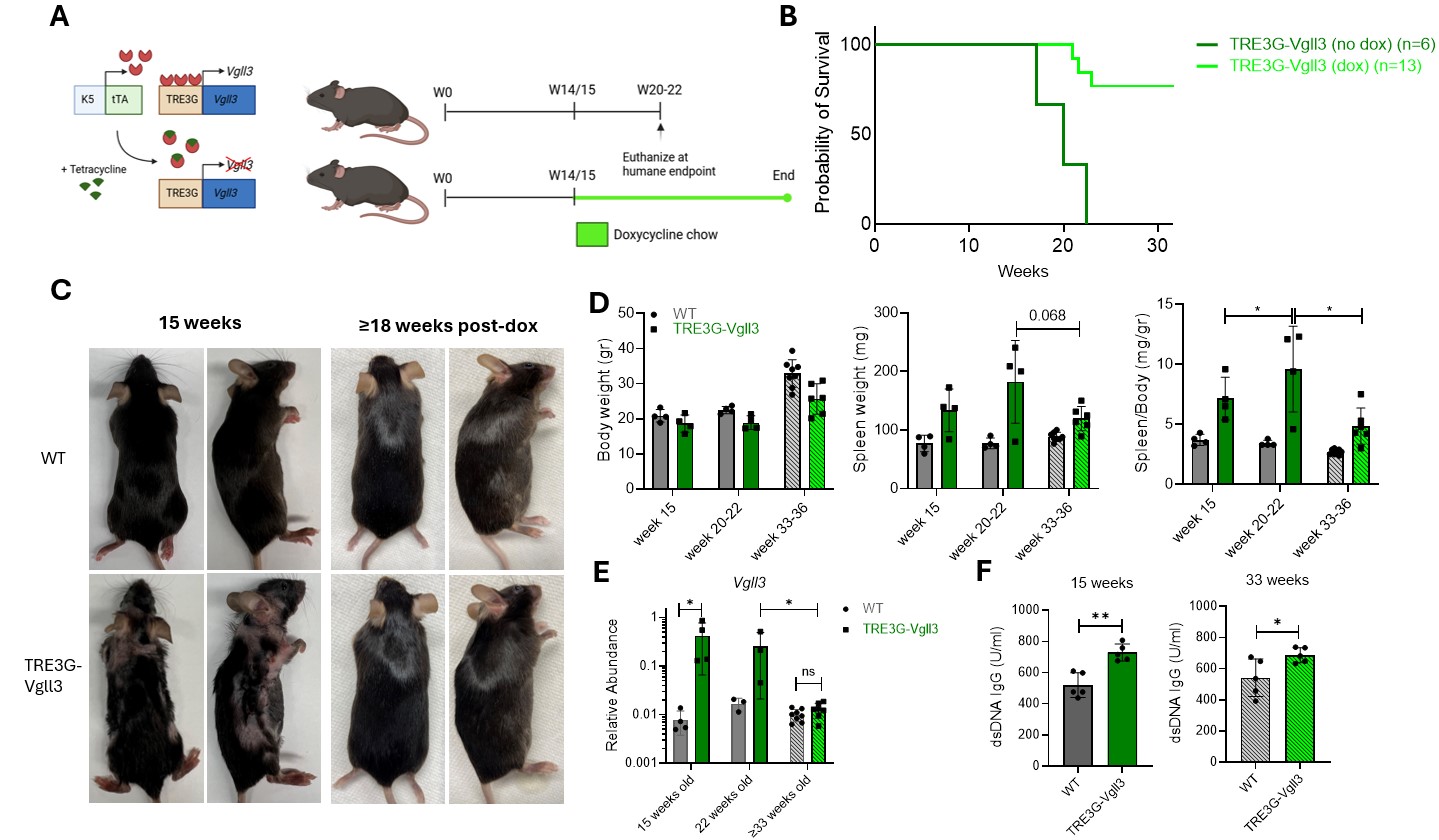 Figure 1: Normalization of epidermal VGLL3 activity ameliorates skin disease and select systemic manifestations. A. Schematic overview of K5-tTAxTRE3G-Vgll3 mouse model and experimental approach. B. Survival curve of mice on and off Doxycycline (dox) chow regimen. C. Gross images of mice at 15 weeks (before dox) and after ≥18 weeks of dox chow. D. Body weights, spleen weights, and spleen/body ratios of mice at 15 and 22 weeks (without dox, solid) and at ≥33 weeks (with dox, dashed). E. RNA expression levels in the same groups. F. Serum anti-dsDNA IgG at 15 weeks and 33 weeks.
Figure 1: Normalization of epidermal VGLL3 activity ameliorates skin disease and select systemic manifestations. A. Schematic overview of K5-tTAxTRE3G-Vgll3 mouse model and experimental approach. B. Survival curve of mice on and off Doxycycline (dox) chow regimen. C. Gross images of mice at 15 weeks (before dox) and after ≥18 weeks of dox chow. D. Body weights, spleen weights, and spleen/body ratios of mice at 15 and 22 weeks (without dox, solid) and at ≥33 weeks (with dox, dashed). E. RNA expression levels in the same groups. F. Serum anti-dsDNA IgG at 15 weeks and 33 weeks.
To cite this abstract in AMA style:
van Drongelen V, Rew J, Griffin E, Young K, Plazyo O, Gharaee-Kermani M, Syu L, Stoll S, Zhou J, Ward N, Kahlenberg J, Tsoi L, Dlugosz A, Gudjonsson J, Billi A. Targeting the Female-biased Factor VGLL3 in Cutaneous and Systemic Lupus [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/targeting-the-female-biased-factor-vgll3-in-cutaneous-and-systemic-lupus/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/targeting-the-female-biased-factor-vgll3-in-cutaneous-and-systemic-lupus/
