Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Some systemic autoimmune rheumatic diseases (SARD), such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE), have been associated with farming, specific pesticides, and other occupational exposures in the Agricultural Health Study (AHS), a prospective cohort of ~89,000 licensed pesticide applicators and spouses in North Carolina and Iowa enrolled in 1993-1997. We previously identified incident RA based on self-report confirmed by DMARD use and case validation, e.g., 220 cases (0.8%) among 26,354 male private pesticide applicators with available follow-up data through 2010. However, incomplete cohort follow-up limits the assessment of disease rates, and many rarer SARD were not included on questionnaires. Thus, we used cohort-linked Medicare claims data to enhance case ascertainment for future analyses of agricultural exposures and risk of SARD.
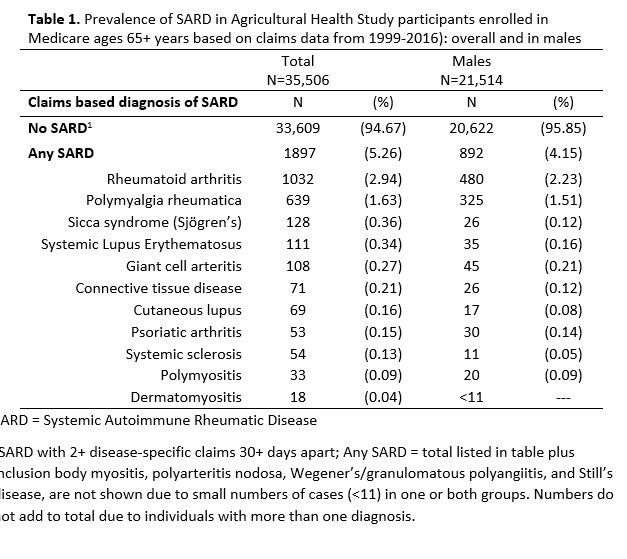
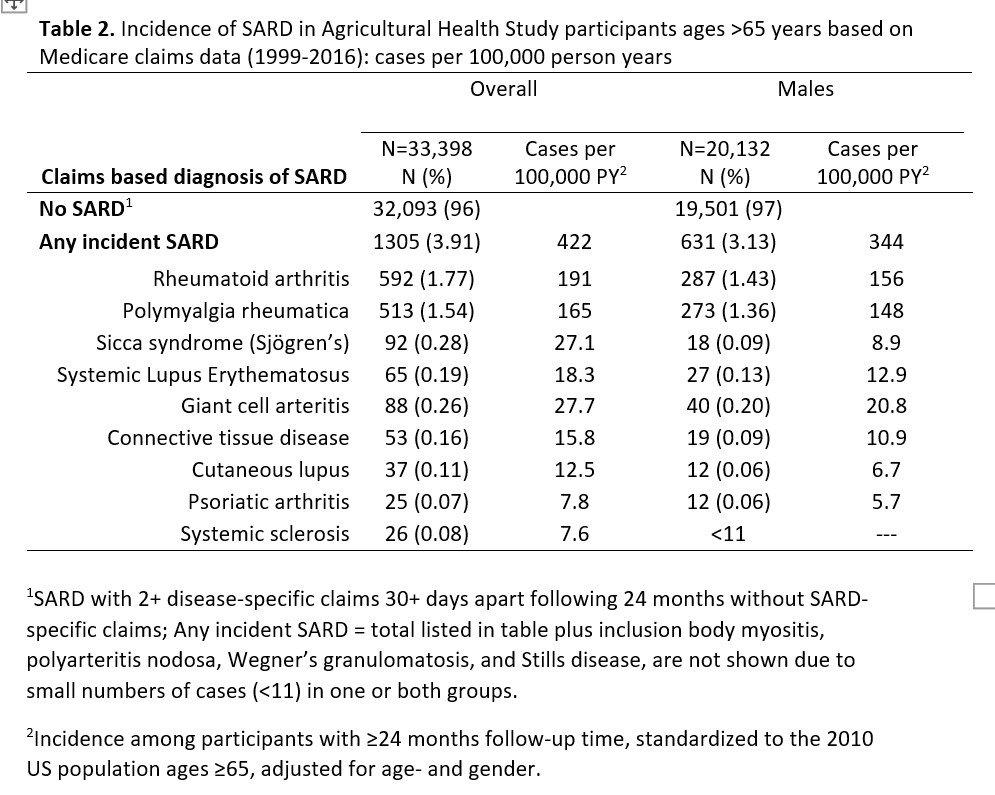
Methods: The AHS cohort includes licensed pesticide applicators (N=52,394 private and 4,916 commercial, 97% male) and spouses (32,345, 99% female). We assessed SARD prevalence based on Medicare claims data from 1999-2016 in 35,506 participants (21,554 male) who enrolled in Medicare at ages ≥65 years with ≥1 year of Fee for Service coverage (FFS; Parts A and B, but not Part C). We sought to identify cases of 15 SARD using ICD codes, requiring ≥2 disease-specific claims ≥30 days apart. In a subset of 33,398 (20,132 male) with a 24-month clean period (i.e., continuous FFS with no SARD-specific claims), we identified incident cases and calculated age- and sex-standardized incidence rates.
Results: Overall, we identified 1987 SARD cases (5.33%), including 892 (4.15%) among males (Table 1). The top 5 diagnoses were rheumatoid arthritis (1,032; 2.90%), polymyalgia rheumatica (PMR, N=639; 1.80%), sicca syndrome (SS, 128; 0.36%), SLE (111; 0.31%), and giant cell arteritis (GCA; 108; 0.30%). Among males, prevalence was slightly lower for RA (480; 2.23%), PMR (325; 1.51%), and GCA (45; 0.21%), and substantially lower for SS (27; 0.12%) and SLE (35; 0.16%). A total of 1305 (3.91%) met the criteria for incident SARD, including 636 (3.13%) male cases, with 287 (1.43%) incident RA, 273 (1.36%) PMR, and the remaining rarer SARD (0-0.20%; Table 2).
Conclusion: In this agricultural cohort, about 1 in 20 older individuals was diagnosed with an SARD based on Medicare claims. Incidence of Medicare-based RA in males was greater than we previously identified by questionnaire. These data will facilitate comparisons of SARD in the AHS with published rates in the Medicare population and will enhance research on the role of pesticides and other exposures in the development of SARD in older AHS participants.
To cite this abstract in AMA style:
Parks C, Costenbader K, Beane Freeman L, Hofmann J, Sandler D. Systemic Autoimmune Rheumatic Diseases (SARD) in the Agricultural Health Study Cohort: Rates of Rheumatoid Arthritis (RA) and Other SARD Among Medicare-linked Participants [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/systemic-autoimmune-rheumatic-diseases-sard-in-the-agricultural-health-study-cohort-rates-of-rheumatoid-arthritis-ra-and-other-sard-among-medicare-linked-participants/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-autoimmune-rheumatic-diseases-sard-in-the-agricultural-health-study-cohort-rates-of-rheumatoid-arthritis-ra-and-other-sard-among-medicare-linked-participants/