Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Salivary gland involvement is a hallmark of disease in primary Sjögren’s syndrome (pSS). This is reflected by the prominent role of a positive biopsy within the ACR-EULAR classification criteria, which is solely based on the focus score (FS). In pSS all salivary glands might be involved in the disease process. For this reason, both labial and parotid salivary gland biopsies can be used for diagnosis and evaluation. Although nearly all clinical centres obtain labial gland biopsies for classification and diagnosis of pSS, a parotid biopsy is also a safe and effective procedure. Furthermore, it has a comparable diagnostic potential in pSS, might be associated with less morbidity, and may even detect presence of subclinical MALT lymphomas. However, histopathological differences between both types of salivary glands should potentially be taken into account.
The aim of this study was to get histopathological insight in minor (labial) and major (parotid) salivary glands in pSS patients in comparison with non-SS sicca patients.
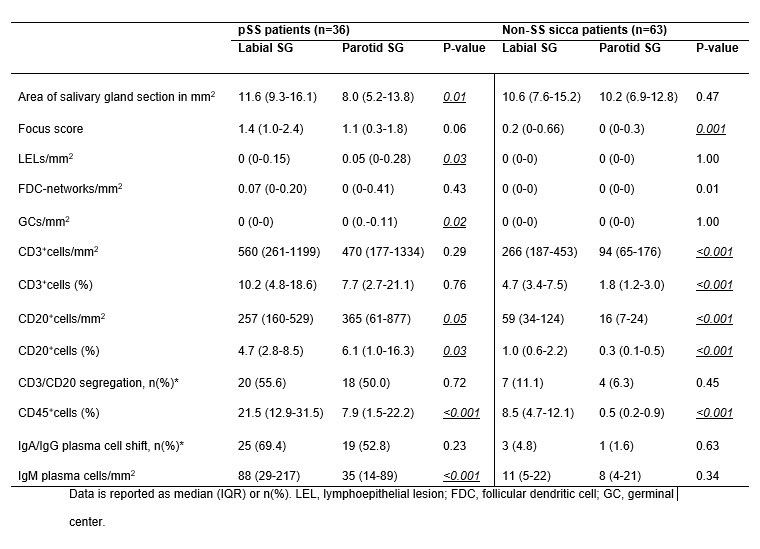
Methods: Both labial and parotid salivary gland biopsies were obtained from 99 patients. According to the expert opinion of three experienced rheumatologists, 36 patients were classified as pSS patients and 63 as non-SS sicca patients. Salivary gland biopsies were formalin fixed, paraffine embedded and serially sectioned at 3-4µm. Sections were stained with H&E and for CD3, CD20, CD45, hmwCK, CD21, Bcl6, IgA/IgG and IgM. Focus score (FS), relative area of lymphocytic infiltrate, level of lymphoid organization and presence of a plasma cell shift were determined. In addition, number of lymphoepithelial lesions, germinal centers, follicular dendritic cell networks, B-cells and T-cells were analyzed.
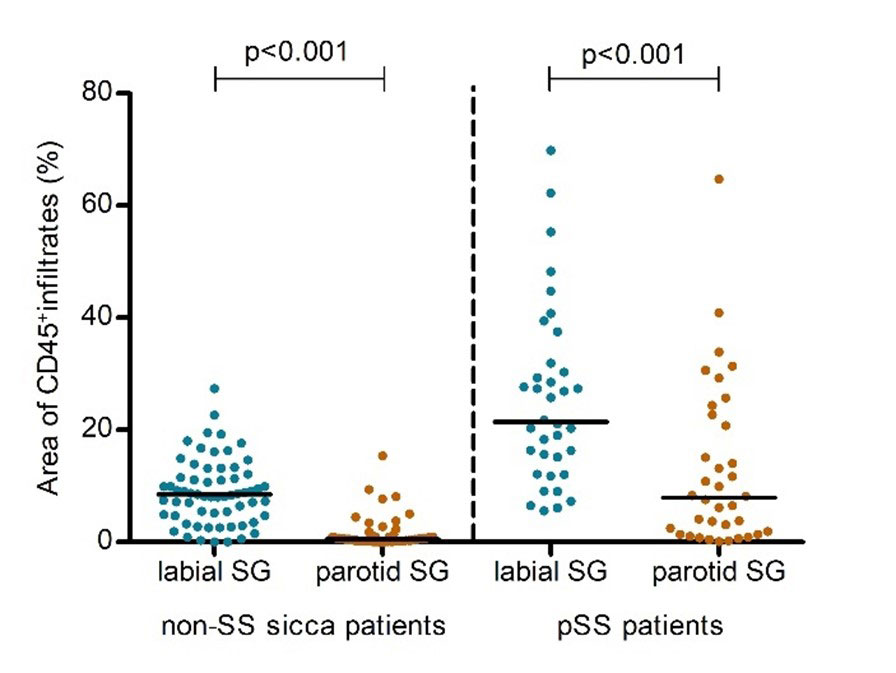
Results: All histopathological parameters differed significantly between pSS and non-SS sicca patients in both labial and parotid salivary gland sections. Comparison of the two salivary gland types of non-SS sicca patients revealed more signs of inflammation in labial gland biopsies as shown by a significantly higher FS, CD3+ T-cells, CD20+ B-cells and relative area of CD45+ infiltrates compared to non-SS parotid salivary gland biopsies. Other histopathological parameters were comparable between the two types of salivary glands. In pSS patients, a higher FS and relative area of CD45+infiltrates was observed in labial gland biopsies compared to parotid gland biopsies. Nevertheless, relative and absolute CD20+ B-cell counts, GCs/mm2 and LELs/mm2 were higher in parotid gland parenchyma.
Conclusion: This study shows in labial salivary gland biopsies of non-SS sicca patients more signs of (unspecific) inflammation compared to parotid biopsies. In parotid gland biopsies signs of B-cell hyperactivity, such as number of CD20+B-cells, GCs/mm2 and LELs/mm2, are more pronounced, compared to labial gland biopsies. These histopathological differences should be taken into consideration in diagnosis and classification of Sjögren’s disease.
To cite this abstract in AMA style:
Nakshbandi U, van Ginkel M, Liefers S, Bootsma H, Spijkervet F, Vissink A, van der Vegt B, Kroese F. Labial and Parotid Salivary Gland Histopathology in Primary Sjögren’s Syndrome [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/labial-and-parotid-salivary-gland-histopathology-in-primary-sjogrens-syndrome/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/labial-and-parotid-salivary-gland-histopathology-in-primary-sjogrens-syndrome/