Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: To evaluate the burden, longitudinal trends, and drivers of multimorbidity (MM; the presence of ≥2 morbidities) in patients with Systemic Sclerosis (SSc) vs. age- and sex-matched non-SSc comparators in a community-based incident cohort.
Methods: A population-based cohort of incident SSc patients from Jan 1, 1980, to Dec 31, 2020, were identified and compared to age- and sex-matched comparators (2:1) from the same population. They were followed till death, migration from the geographic area, or Sept. 30, 2022. Data on 21 morbidities identified by the US Department of Health and Human Services (DHHS) and 13 morbidities in the Charlson Comorbidity Index (CCI) was retrieved. Cumulative incidence of MM (MM2+) or substantial MM (MM5+; ≥ 5 morbidities) adjusting for the competing risk of death was estimated. Cox models adjusted for age, sex, index year and morbidity count at index date were used to compare cases and comparators. Patients with < 1 year of prior medical history and who met the criteria of event type before the index date were excluded.
Results: We included 189 SSc patients and 408 comparators (mean age 58.2 y, 85% female, 91% white).
The prevalence of cardiac arrhythmia (19% vs 10%, p=0.002), arthritis (34% vs 22%, p=0.002), COPD (12% vs 5%, p=0.007), MI (3% vs 0%, p=0.023), peripheral vascular disease (33% vs 4%, p< 0.001), chronic pulmonary disease (19% vs 13%, p=0.035), and any liver disease (5% vs 2%, p=0.032) were higher at index date, but the prevalence of hyperlipidemia (30% vs 39%, p=0.043) was lower in SSc.
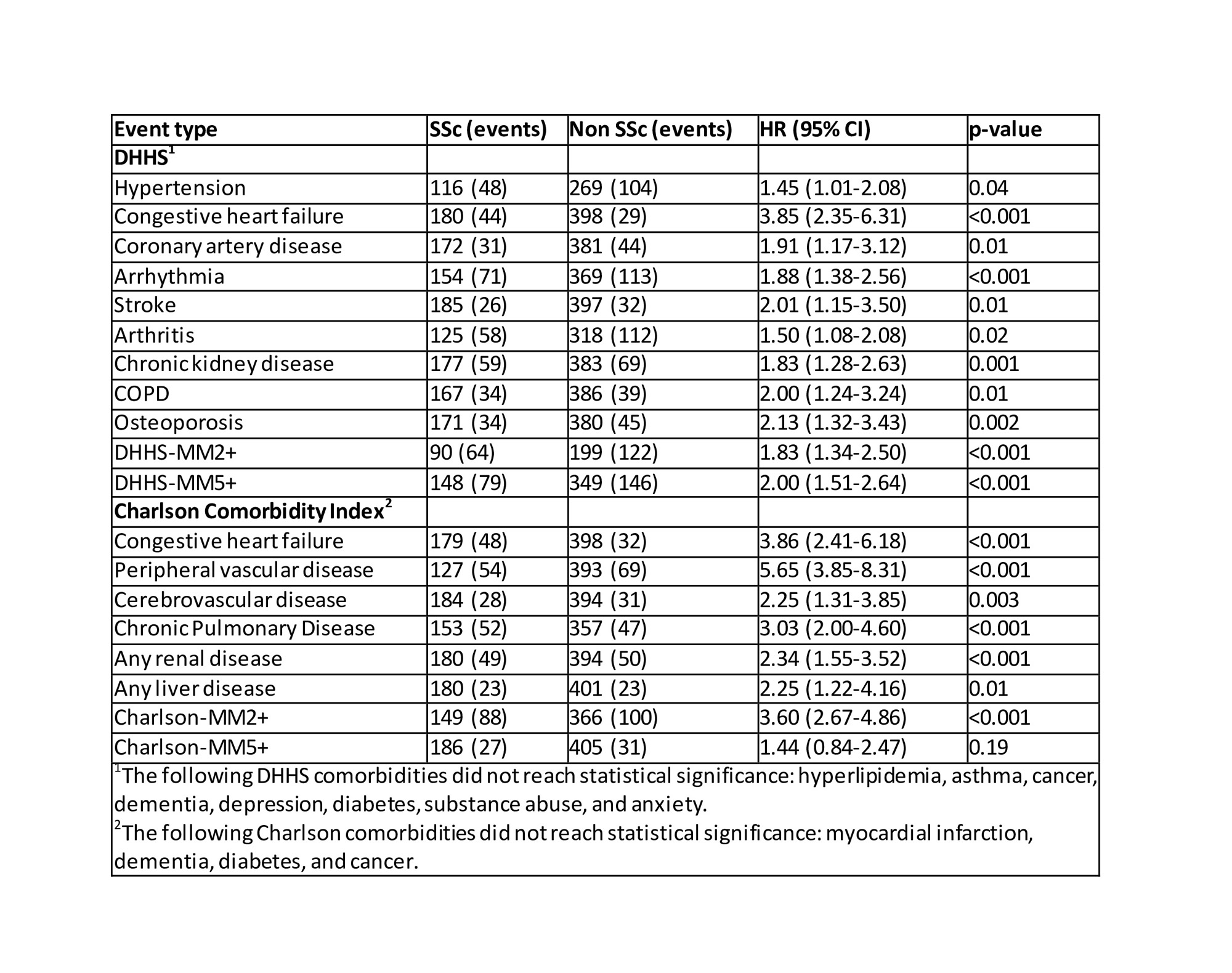
During a mean length of follow-up of 9.7 y (SD 8.7) for non-SSc and 8.5 y (SD 8.0) for SSc, the development of hypertension (HR 1.45; 95% CI 1.01-2.08), congestive heart failure (DHHS: HR 3.85, 95% CI 2.35-6.31; CCI: HR 3.86, 95% CI 2.41-6.18), coronary artery disease (HR 1.91, 95% CI 1.17-3.12), arrhythmia (HR 1.88, 95% CI 1.38-2.56), stroke (HR 2.01, 95% CI 1.15-3.50), arthritis (HR 1.50, 95% CI 1.08-2.08), chronic kidney disease (HR 1.83, 95% CI 1.28-2.63), COPD (HR 2.00, 95% CI 1.24-3.24), osteoporosis (HR 2.13, 95% CI 1.32-3.43), peripheral vascular disease (HR 5.65, 95% CI 3.85-8.31), cerebrovascular disease (HR 2.25, 95% CI 1.31-3.85), chronic pulmonary disease (HR 3.03, 95% CI 2.00-4.60), any renal disease (HR 2.34, 95% CI 1.55-3.52), and any liver disease (HR 2.25, 95% CI 1.22-4.16) were significantly higher in SSc when compared to non-SSc. (Table 1)
The risk of development of DHHS MM2+, DHHS MM5+, and CCI-MM2+ was significantly higher in SSc patients vs non-SSc, but CCI-MM5+ was statistically insignificant after adjusting for baseline morbidity count. (Figure 1 and Table 1)
Conclusion: There is a high burden of MM and substantial MM in SSc patients at baseline and during the disease course.Witha1.5-4-fold risk of development of cardiopulmonary diseases, 2-fold risk of neurological, renal and liver diseases, and 6-fold risk of peripheral vascular disease in SSc patients during follow-up, there is an urgent need for systematic assessment and management of multimorbidity to reduce healthcare burden and improve prognosis in this population.
To cite this abstract in AMA style:
Karn A, Achenbach S, Hinze A, Crowson C, Makol A. Incidence, Trends, and Determinants of Multimorbidity in Systemic Sclerosis: Data from a Population-based Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/incidence-trends-and-determinants-of-multimorbidity-in-systemic-sclerosis-data-from-a-population-based-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/incidence-trends-and-determinants-of-multimorbidity-in-systemic-sclerosis-data-from-a-population-based-cohort/