Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Guidelines recommend 150 minutes a week in moderate-intensity physical activity (MPA) to improve health in individuals with chronic disease such as those with lumbar spinal stenosis (LSS). LSS affects older adults’ physical function and limits their mobility, which leads to reduced activity participation that might result in further disability. Because of the anatomical changes found in LSS and symptoms presented by patients, health professionals are hesitant in promoting MPA as they are fearful of worsening the condition. Therefore, it is imperative to understand whether MPA affects the concentration of plasma biomarkers in individuals with LSS. Our study aimed to determine the associations between MPA and concentration of plasma biomarkers (i.e., cartilage degeneration and inflammation) in individuals with LSS, and to also explore associations between changes in MPA and changes in concentration of biomarkers.
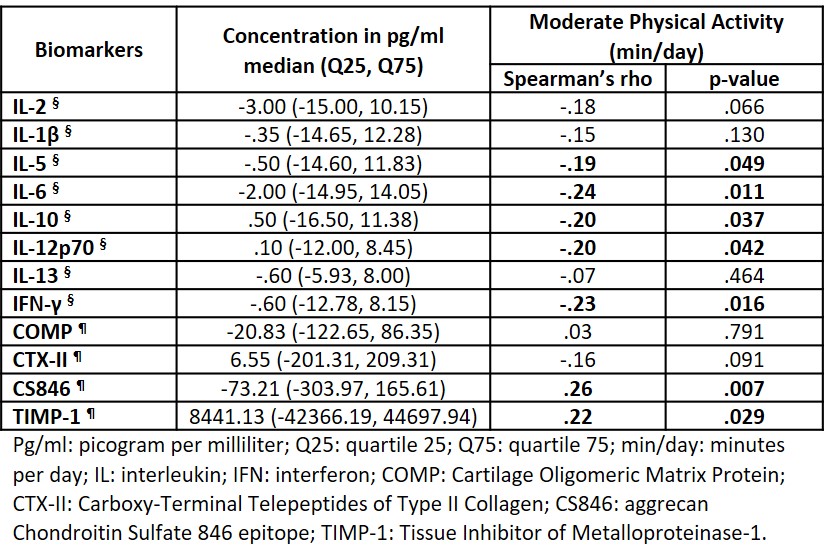
Methods: We performed a secondary analysis from a randomized trial that compared three non-surgical approaches to manage LSS. Participants with available blood samples and MPA measured at baseline and 2-month follow-up were included (N=109). Cartilage degradation was assessed by analyzing the concentration (volume expressed in pg/ml) of different biomarkers (COMP, CTX-II, CS864 and TIMP-1) using enzyme-linked immunosorbent assay kits specific to each biomarker. A panel of 8 inflammatory biomarkers (interleukin [IL]-1β, IL-2, IL-5, IL-6, IL-10, IL-12p70, IL-13 and IFN-γ) were assessed using a MILLIPLEX® MAP Human High Sensitivity T Cell Magnetic Bead Panel. Daily time (min/day) in MPA was assessed using the Sensewear Armband activity monitor for 7 days. Changes (i.e. follow-up minus baseline) in concentration of each biomarker and MPA were calculated. Associations between changes in concentration of biomarkers and in MPA were computed as Spearman’s rho with an alpha of .05. Statistical analyses were performed using IBM SPSS Statistics 26 (IBM Corp, Armonk, NY, USA).
Results: Participants were 52% female, 72.9±7.5 years old, with a BMI of 29.7±5.8. They barely changed their time in MPA from baseline to 2-month follow-up (-4.4±30.8 min/day; median [Q25, Q75] = 0.0 [-8.5, 5.5] min/day). This change in MPA was inversely associated with changes in concentration of inflammatory biomarkers: IL-5 (rho=-.19; p=.049), IL-6 (rho=-.24; p=.011), IL-10 (rho=-20; p=.037), IL-12p70 (rho=-.20; p=.042), IFN-γ (rho=-.23; p=.016); and directly associated with changes in concentration of cartilage degradation biomarkers (pg/ml): CS864 (rho=.26; p=.007) and TIMP-1 (rho=.22; p=.029).
Conclusion: This exploratory analysis in individuals with LSS showed a trend indicating that increases in time spent in MPA may reduce inflammation, however, it may increase cartilage degradation. Promoting MPA in those with LSS may be challenging as few individuals engage in it and the benefit/risk ratio in terms of disease modulation needs further investigation.
To cite this abstract in AMA style:
Almeida G, Khoja S, Terhorst L, Sowa G, Piva S, Schneider M. Effect of Physical Activity on Cartilage Degradation and Inflammation in Individuals with Lumbar Spinal Stenosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/effect-of-physical-activity-on-cartilage-degradation-and-inflammation-in-individuals-with-lumbar-spinal-stenosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/effect-of-physical-activity-on-cartilage-degradation-and-inflammation-in-individuals-with-lumbar-spinal-stenosis/