Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Rosai-Dorfman Disease (RDD), formerly known as sinus histiocytosis with massive lymphadenopathy, was initially thought to be inflammatory or autoimmune in nature. The discovery of MAP-ERK pathway mutations has since reclassified RDD as a histiocytic neoplasm. However, autoimmune diseases have been commonly reported, and recent consensus guidelines recognize “immune-related RDD” as a distinct subtype. Given its clinical overlap with autoimmune diseases, a deeper understanding of RDD’s immunologic profile is increasingly important for rheumatologists.
Methods: We performed a retrospective chart review of histologically confirmed RDD cases from five international referral centers. Using a standardized data collection form, we gathered data on patient demographics, patterns of organ involvement, driver mutations, autoimmune serologies, and treatment outcomes of autoimmune diseases.
Results: We identified 162 patients with RDD diagnosed from Jan 2003- Jan 2025. Median age at diagnosis was 48 years (range, 7-85) with nine patients diagnosed before age 18. Cohort was 64.8% female and racial distribution was 34.6% Black, 33.3% White, and 24.7% Asian (Table 1). Multisystem involvement was noted in 53.7% of cases, with common sites including skin/subcutaneous tissue (49.4%), lymph nodes (39.5%), and bone (33.9%). Autoimmune diseases were present in 29 patients (17.9%), among which, the most common were systemic lupus erythematosus (6, 20.7%) and rheumatoid arthritis (5, 17.2%) (Figure 1). Autoimmune disease was more frequent in multisystem vs single organ RDD (62% vs 38%, p=0.3). Mean ESR and CRP were higher in patients with autoimmune disease (37.1 mm/Hr and 53.5 mg/L) vs patients without autoimmune disease (25.5 mm/Hr and 39.4 mg/L). Autoantibodies were detected in 44 of 94 tested (46.8%), most commonly ANA in 33.3% (29/87) (Figure 2). Tissue-based next generation sequencing was performed in 102 patients (62.9%), revealing KRAS mutation (11.7%), MEK mutations (9.3%), other mutations (16.7%) and no mutation (25.3%). No significant association was observed between mutational status and autoimmunity. Autoimmune disease preceded RDD diagnosis in 19 cases (11.7%). Treatment data were available for 22 of 29 patients with autoimmune disease: 11 (50%) were stable off treatment, 10 (45.5%) were stable on DMARD therapy, and 1 (4.5%) had active disease despite multiple DMARDs. Median follow-up for the entire cohort was 29.8 months (IQR 10.4–61.4). Eight deaths were reported in the cohort, none among patients with autoimmune disease.
Conclusion: This multi-center cohort highlights the clinical and molecular diversity of RDD. It also reveals a high prevalence of autoimmunity in RDD, both in terms of autoimmune disease (17.9 %) and positive autoantibodies (46.8 %), which is higher than general population rates of approximately 3% and 16% respectively. There was a trend toward association of autoimmune disease with multisystem RDD and with higher inflammatory markers at the time of RDD diagnosis. Overall, findings highlight the need for investigation into shared pathogenesis and potential therapeutic strategies that could target both RDD and autoimmune diseases.
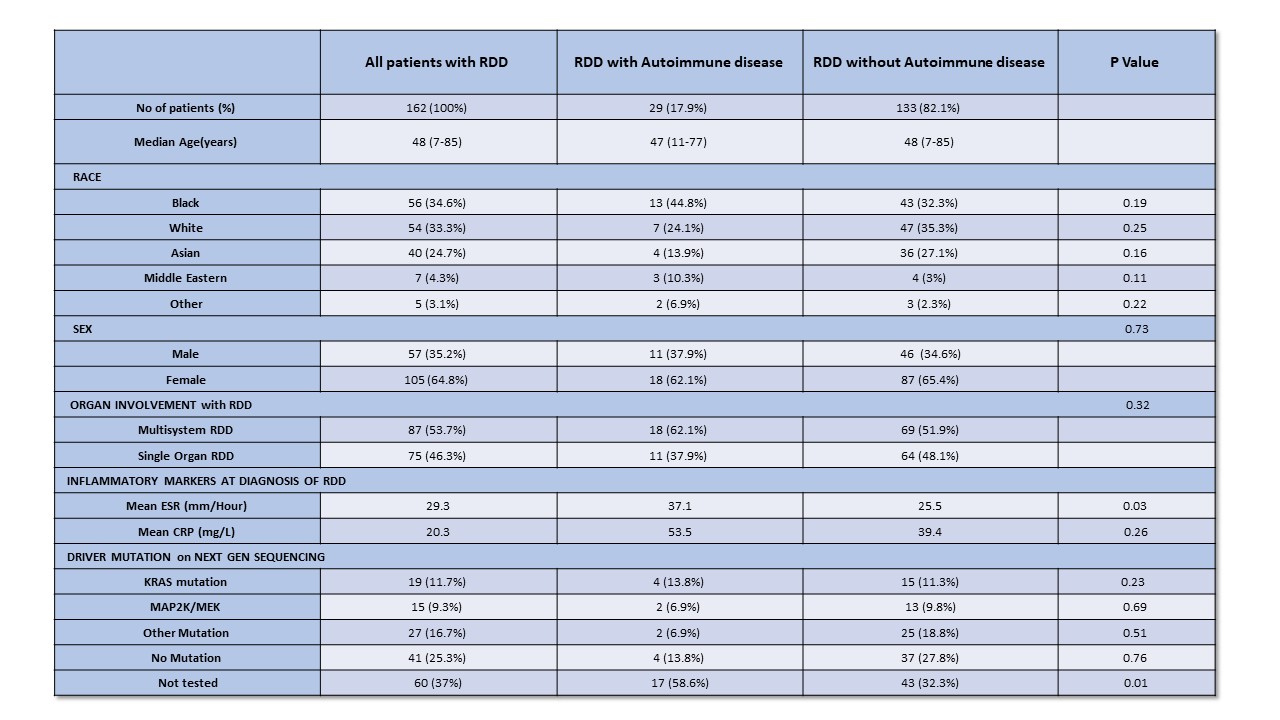 Characteristics of individuals with RDD and Autoimmune disease
Characteristics of individuals with RDD and Autoimmune disease
.jpg) List of autoimmune diseases seen in patients with RDD (no of patients)
List of autoimmune diseases seen in patients with RDD (no of patients)
.jpg) Autoantibodies in patients with RDD (% of patients positive)
Autoantibodies in patients with RDD (% of patients positive)
To cite this abstract in AMA style:
Sen M, Ruan G, Reynolds S, Ali H, Yang X, Morlote D, Ravindran A, Shea L, Koster M, Abeykoon J, Salama H, Cao X, Ahmed A, Go R, Goyal G. High Prevalence of Autoimmunity in Rosai Dorfman Disease: A Multinational Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/high-prevalence-of-autoimmunity-in-rosai-dorfman-disease-a-multinational-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-prevalence-of-autoimmunity-in-rosai-dorfman-disease-a-multinational-study/
