Session Information
Date: Monday, November 13, 2023
Title: (1221–1255) Pediatric Rheumatology – Clinical Poster II: Connective Tissue Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) is associated with significant morbidity and mortality. The 2018 International Society of Nephrology/Renal Pathology Society (ISN/RPS) classification criteria and the NIH chronicity activity indices are used for LN classification. Some adult studies report tubulointerstitial (TI) inflammation is an independent predictor of renal outcomes in LN. However, its impact in pediatric LN remains unexplored.
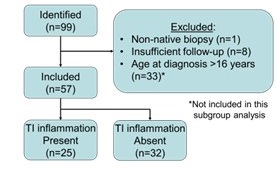
Methods: We conducted a retrospective, observational cohort study utilizing a subgroup analysis of patients with biopsy-confirmed LN. Inclusion criteria encompassed all patients with biopsy-confirmed lupus nephritis, where the renal biopsies were performed at the University of Chicago between January 1, 2006, and September 6, 2022. Patients were required to be ≤ 21 years of age at the time of their initial kidney biopsy. Exclusion criteria consisted of a follow-up duration of ≤ 3 months and an age ≥ 16 years at the time of initial lupus diagnosis. Non-native renal biopsies were also excluded. The primary outcome measures were end-stage renal disease (ESRD) and/or the need for dialysis.
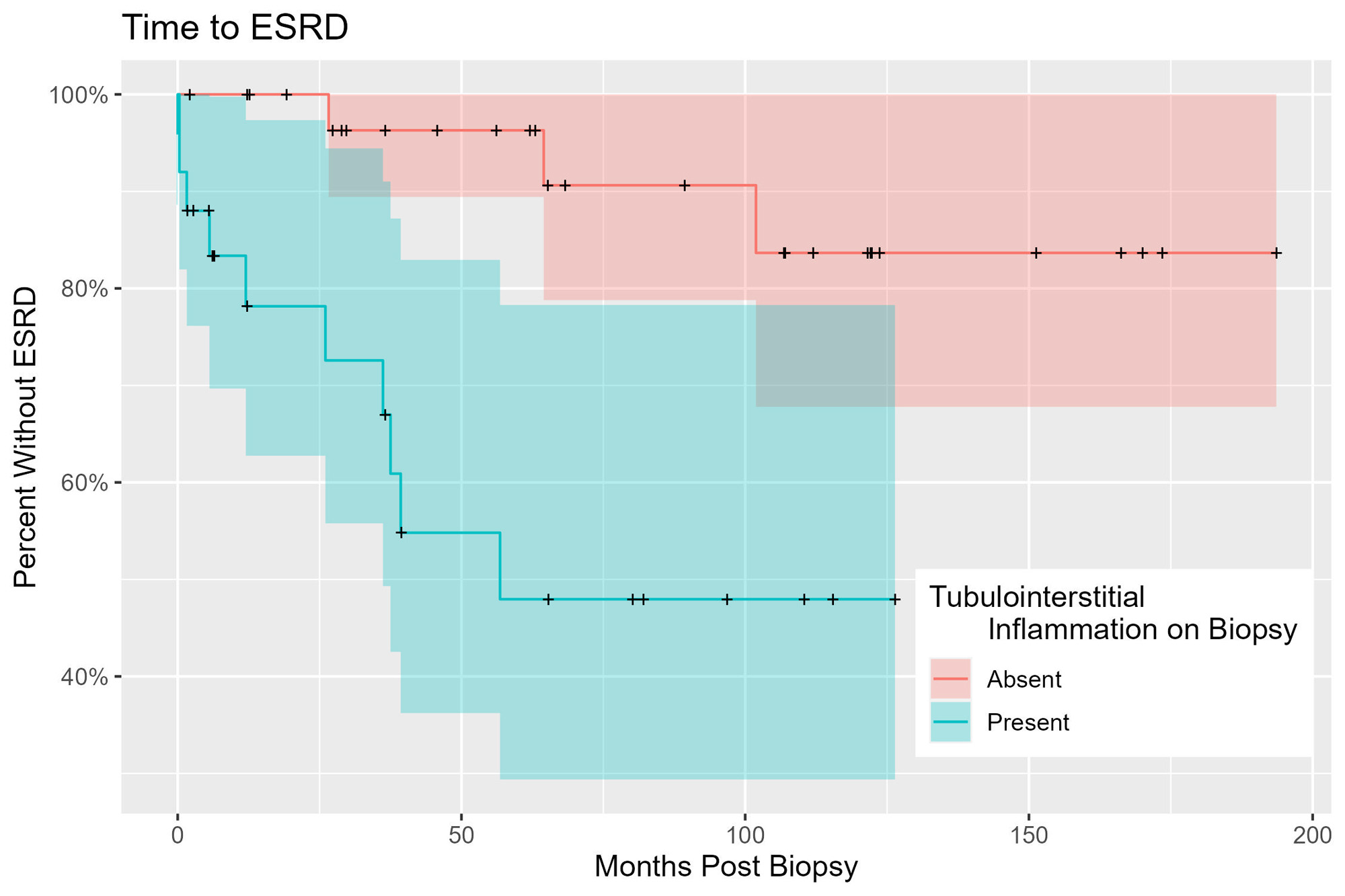
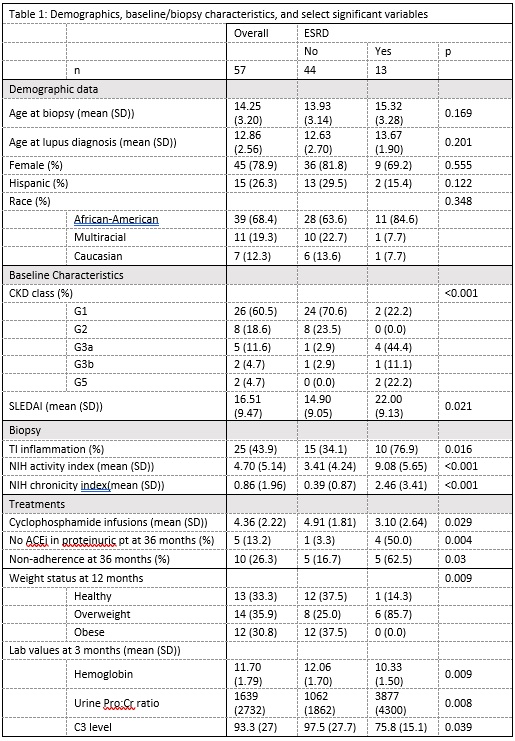
Results: Out of 99 identified biopsies, 42 were excluded, leaving 57 patients for analysis (see figure 1). The mean follow-up duration was 74 months (SD 26, max 210). TI inflammation was present for 25 (44%) and absent for 32 (56%). Of those with TI inflammation, 10 (40%) developed ESRD while only 3 (9.4%) without inflammation developed ESRD. Survival analysis showed a significant association with ESRD, with a positive likelihood ratio of 6.6 (95% CI 1.8, 24.3). Patients with TI inflammation experienced a shorter time to ESRD (mean 21.51 months, SD 20.32) compared to those without TI inflammation (mean 64.33 months, SD 37.65; see figure 2). ESRD was correlated with the NIH activity index (LR 1.9, 95% CI 1.1 – 1.3) and the NIH chronicity index (LR 3.1, 95% CI 1.8 – 5.4). Hemoglobin, C3 level, and proteinuria at 3 months and obesity at 12 months was associated with ESRD. ESRD was not correlated with ISN/RPS classification, race, sex, Hispanic ethnicity, or induction treatment (see table 1). It should be noted that 35 patients (62%) had missing data for non-outcome variables at certain timepoints. This study had a considerable amount of missing data for non-outcome variables, leading to wide confidence intervals due to the high proportion of right-censored data and limited number of events.
Conclusion: Our findings indicate a significant association between tubulointerstitial (TI) inflammation and the primary endpoint of ESRD or dialysis in our pediatric lupus nephritis cohort. Further evaluation of TI inflammation may provide valuable insights into the pathogenesis, prognosis, and treatment of pediatric lupus nephritis patients. However, these conclusions are constrained by the retrospective nature of the study and the significant amount of missing data.
To cite this abstract in AMA style:
Mitacek R, Liu Q, Wagner-Weiner L, Hashmat S, Chang A. Tubulointerstitial Inflammation Is Associated with End-Stage Renal Disease in Pediatric Lupus Nephritis: A Single Center Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/tubulointerstitial-inflammation-is-associated-with-end-stage-renal-disease-in-pediatric-lupus-nephritis-a-single-center-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/tubulointerstitial-inflammation-is-associated-with-end-stage-renal-disease-in-pediatric-lupus-nephritis-a-single-center-retrospective-cohort-study/