Session Information
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Juvenile dermatomyositis (JDM) is a systemic vasculopathy associated with metabolic derangements and possible increased risk for premature atherosclerosis. Oxidation of low-density lipoprotein (LDL) in the endothelial wall of blood vessels is an early step in atherosclerotic plaque formation. The primary aim of this study was to compare deposition of oxidized LDL in the vasculature of muscle biopsies (MBx) from patients with untreated JDM compared to pediatric controls.
Methods: After informed consent, MRI-directed MBx were obtained from 20 female patients with JDM (mean age = 6.3+/-2.2) before the start of therapy and 5 female controls (mean age = 14.4+/-1.8). Frozen muscle sections were stained with DAPI and fluorescently labeled antibodies against von Willebrand factor (vWF) and LDL oxidized by copper (oxLDL) and were imaged by a Leica DMR-HC upright microscope. ImageJ (NIH, Bethesda, MD) was used to identify blood vessel areas, defined by the presence of vWF, and measure the fluorescence of the area and intensity of oxLDL within the vessel walls. For each vessel visualized, the intensity of oxLDL was calculated for the area of the vessel and corrected for background intensity. The total fluorescence for each muscle biopsy was calculated by dividing the sum of the intensities of the individual vessels by the sum of the area of the vessels. Data was analyzed using t-tests and Pearson correlation.
Results: Children with untreated JDM demonstrated higher fluorescence of oxLDL in the walls of muscle vasculature compared to healthy children (p=0.03, Figure 1). Secondary analysis revealed significantly higher oxLDL fluorescence in muscle biopsies of patients with the TNF-a-308 G allele compared to biopsies of patients with the A allele (p=0.04, Figure 2). Within the JDM cohort, there was a trend towards increased oxLDL fluorescence with longer duration of untreated disease at time of MBx. There was no significant correlation found between oxLDL fluorescence and markers of disease activity including disease activity (DAS) scores, nailfold capillary end row loops, muscle enzymes, serum vWF antigen, or neopterin.
Conclusion: Increased deposition of oxLDL within blood vessels of children with JDM supports the concern that these children are at increased risk for premature atherosclerosis. Additional longitudinal studies are needed to better understand the long term impact on morbidity and mortality.
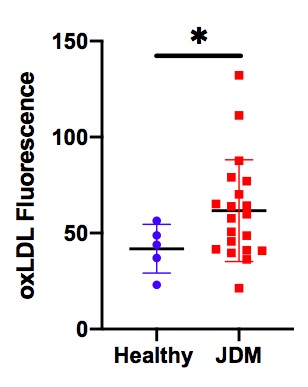 Figure 1: Fluorescence of oxLDL (intensity/area) in the walls of muscle vasculature is increased in JDM muscle biopsies compared to healthy controls (p=0.03). The mean value is indicated by the line, and the standard deviation is indicated by the whiskers. JDM patients, n=20, and healthy controls, n=5.
Figure 1: Fluorescence of oxLDL (intensity/area) in the walls of muscle vasculature is increased in JDM muscle biopsies compared to healthy controls (p=0.03). The mean value is indicated by the line, and the standard deviation is indicated by the whiskers. JDM patients, n=20, and healthy controls, n=5.
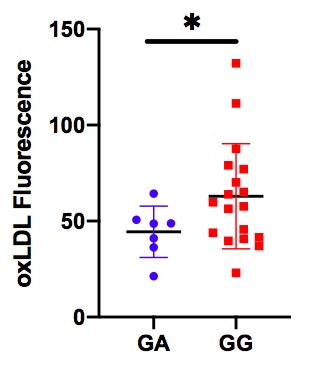 Figure 2: Fluorescence of oxLDL (intensity/area) in the walls of muscle vasculature is increased in subjects with the GG polymorphism at the TNFa_308 gene locus compared to subjects with the GA polymorphism (p=0.04).
Figure 2: Fluorescence of oxLDL (intensity/area) in the walls of muscle vasculature is increased in subjects with the GG polymorphism at the TNFa_308 gene locus compared to subjects with the GA polymorphism (p=0.04).
To cite this abstract in AMA style:
Spitznagle J, Kacha-Ochana A, Cook-Mills J, Khojah A, Morgan G, Pachman L. Vascular Deposition of Oxidized LDL Is Increased in Children with Untreated Juvenile Dermatomyositis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/vascular-deposition-of-oxidized-ldl-is-increased-in-children-with-untreated-juvenile-dermatomyositis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vascular-deposition-of-oxidized-ldl-is-increased-in-children-with-untreated-juvenile-dermatomyositis/
