Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: The FRAX tool, launched by the World Health Organization Collaborating Centre at the University of Sheffield in 2008 (https://www.sheffield.ac.uk/FRAX/), is widely used to quickly and reliably estimate an individual’s fracture risk, outputting the ten-year probability of major osteoporotic fracture (thoracic/lumbar vertebra, proximal femur, distal forearm, or proximal humerus) and the ten-year probability of hip fracture. The FRAX algorithm accounts for the influence of several risk factors, including rheumatoid arthritis (RA), as individuals with RA are known have an excess burden of fractures. However, the use of FRAX specifically within RA populations to estimate fracture risk has not been widely studied. Therefore, the purpose of this study was to determine the accuracy of FRAX risk predictions for US individuals with RA.
Methods: In this retrospective cohort study, all patients aged 40-90 years within a geographically defined region who fulfilled the 1987 American College of Rheumatology criteria for RA from 1980 to 2007 were identified and followed until death, migration, or last medical record review. Each RA patient was matched 1:1 on age and sex to a patient of the same region without RA. The date of RA criteria fulfillment served as the baseline date for RA patients and matched subjects. Ten-year predictions for major osteoporotic and hip fractures were estimated using the FRAX tool. FRAX prediction scores (without bone mineral density) were calculated from patient age, sex, body mass index, and the following dichotomous risk factors: RA, previous fracture, secondary osteoporosis, glucocorticoid use, smoking status, and alcohol use. Fractures were ascertained through follow-up, truncated at 10 years. Standardized incidence ratios (SIR) and 95% confidence intervals (CI) were calculated to compare observed and predicted fractures.
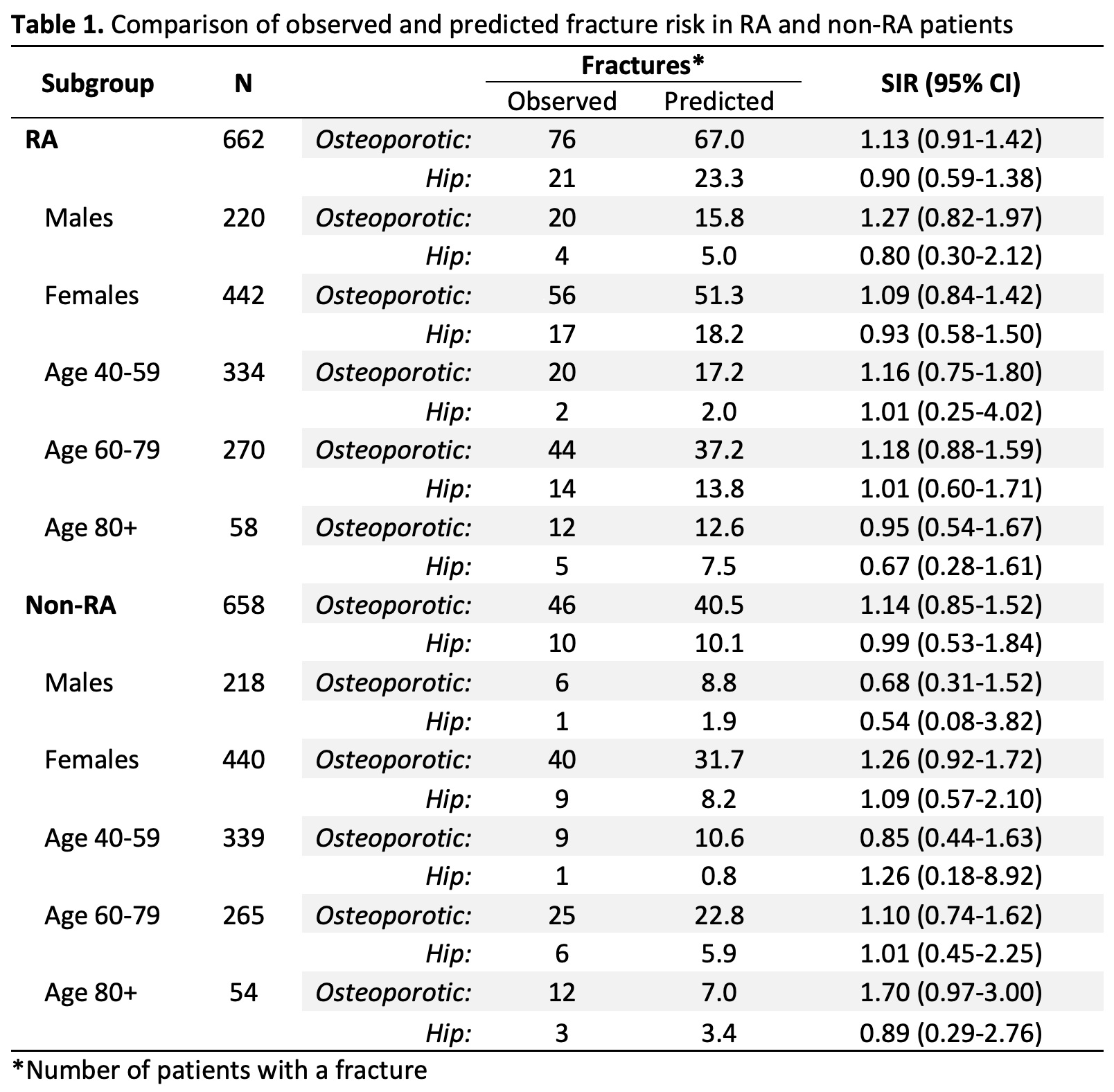
Results: The study included 662 RA patients and 658 non-RA comparators. RA and non-RA subjects were predominantly white females (67% female; RA: 95% white, non-RA: 94% white) with a mean age of 60.6 and 60.5 years at baseline, respectively. Individuals with RA had increased occurrence of all other dichotomous risk factors compared to non-RA comparators, with the exception of previous fractures, which was similar between RA and non-RA groups. Among RA patients, 76 major osteoporotic and 21 hip fractures were observed during follow-up (median follow-up: 9.7 years, IQR: 5.7, 10.0 years) compared to the predicted 67.0 major osteoporotic fractures (SIR: 1.13, 95% CI: 0.91-1.42) and 23.3 hip fractures (SIR: 0.90, 95% CI: 0.59-1.38). The observed and predicted major osteoporotic and hip fracture risks were similar for RA and non-RA patients, with no significant differences among sex and age subgroups. For non-RA patients over the age of 80 years, the observed risk for major osteoporotic fracture was slightly elevated (SIR: 1.70, 95% CI: 0.97-3.00), but this difference did not reach significance.
Conclusion: The findings of this study support that the FRAX tool is an accurate method for estimating major osteoporotic and hip fracture risk in individuals with RA.
To cite this abstract in AMA style:
Peterson M, Crowson C, Myasoedova E, Amin S, Davis J, Achenbach S, Kholsa S, Atkinson E. Validating the FRAX Score in a US Population-Based Study of Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/validating-the-frax-score-in-a-us-population-based-study-of-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/validating-the-frax-score-in-a-us-population-based-study-of-patients-with-rheumatoid-arthritis/