Session Information
Date: Sunday, November 12, 2023
Title: Abstracts: RA – Treatments I: Novel RA Treatments & Mechanisms of Action
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: Vagus nerve stimulation (VNS) is an emerging potential therapy for rheumatoid arthritis (RA). Given preliminary benefit observed with VNS in RA, we hypothesized that vagotomy might increase the risk of developing RA, without impacting the risk of developing osteoarthritis (OA). Historically, patients underwent vagotomy to treat refractory peptic ulcer disease by one of three methods: 1) full truncal vagotomy, 2) selective vagotomy (in which the celiac branch remains intact), and 3) superselective vagotomy (in which only the direct vagal inputs to the stomach are affected). The aim of this study was to examine the risk of developing RA or OA after various methods of vagotomy.
Methods: We performed a population-based cohort study in Denmark utilizing the Danish National Patient Registry and Danish Civil Registration System (CRS) from January 1, 1977 to December 31, 1995. We identified individuals who underwent vagotomy using International Classification of Diseases (ICD)-8 codes. A comparison cohort of patients who had not undergone vagotomy was randomly selected from the general population and matched on year of birth, sex, and date of vagotomy (index date). We excluded patients who were not registered in the CRS at least two years before the index date and those with prior diagnoses of OA or RA at any time before the index date. We examined the incidence of RA or OA based on two or more diagnosis codes for RA or OA 7-365 days apart, as well as OA with joint replacement based on a diagnosis of OA and a procedure code for knee or hip arthroplasty. Incidence of RA and OA was calculated using cumulative incidence function and treating death as a competing event. We used Cox proportional hazards regression models to compute hazard ratios (HRs) adjusted for age, sex, and comorbidities and corresponding 95% CIs, comparing patients with truncal vagotomy versus a matched general population comparison cohort and superselective vagotomy versus a matched comparison cohort.
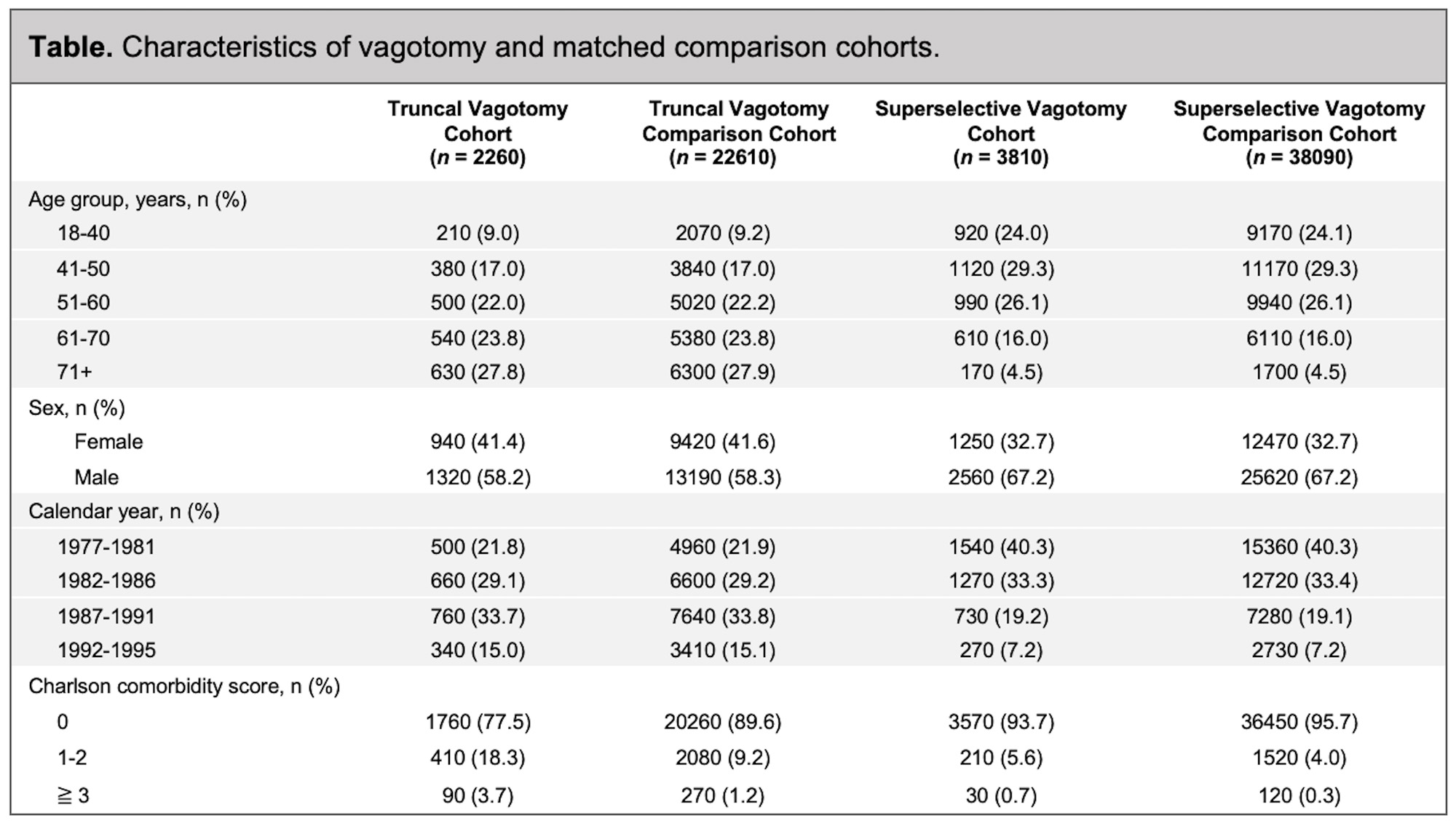
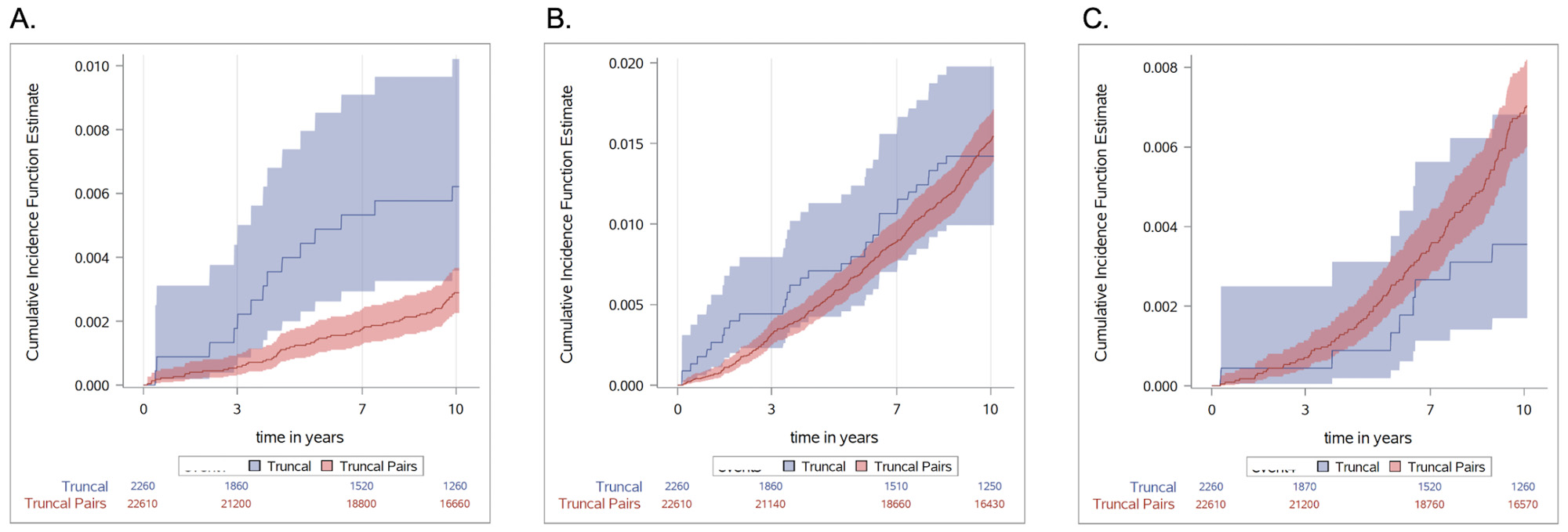
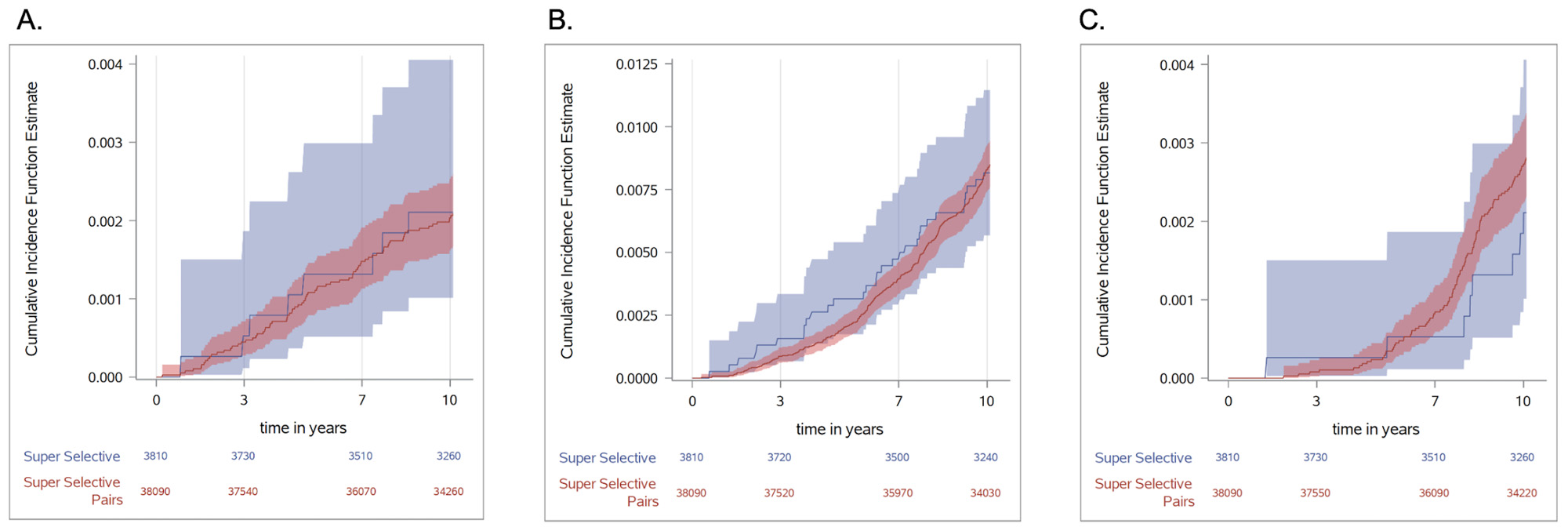
Results: We identified 2,260 patients who underwent truncal vagotomy, matched with 22,610 comparators (Table), as well as 3,810 superselective vagotomy patients matched with 38,090 comparators (Table). The cumulative incidence estimates for truncal vagotomy are shown in Figure 1 and for superselective vagotomy in Figure 2. After adjusting for confounders, the HR for developing RA was 2.62 (95% CI 1.47-4.67) among patients who underwent truncal vagotomy compared with matched pairs. The HR for OA was 1.23 (95% CI 0.86-1.78), and for OA with joint replacement it was 0.73 (95%CI 0.36-1.50). For superselective vagotomy patients compared with a general population comparison cohort, the HR for developing RA was 1.05 (95% CI 0.51-2.17), for OA it was 1.01 (95% CI 0.70-1.45), and for OA with joint replacement it was 0.73 (95% CI 0.36-1.50).
Conclusion: Truncal vagotomy was associated with an increased risk of developing RA. No difference in the risk of RA was seen in the superselective vagotomy group. Neither truncal nor superselective vagotomy were associated with an increased risk of developing OA. These results support the hypothesis that disruption of vagus nerve signaling may contribute to the development of RA.
To cite this abstract in AMA style:
Baker M, Nagy D, Tamang S, Horváth-Puhó E, Toft Sørensen H. Vagotomy and Subsequent Risk of Rheumatoid Arthritis and Osteoarthritis: A Danish Register-Based Cohort Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/vagotomy-and-subsequent-risk-of-rheumatoid-arthritis-and-osteoarthritis-a-danish-register-based-cohort-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/vagotomy-and-subsequent-risk-of-rheumatoid-arthritis-and-osteoarthritis-a-danish-register-based-cohort-study/