Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: With the current workforce shortage, wait times for initial consultation with pediatric rheumatology are lengthy and many referrals do not result in a rheumatic diagnosis. This study aims to develop a predictive algorithm for diagnosis of inflammatory arthritis and systemic lupus erythematosus (SLE) by utilizing patient-reported, historical, and referral data obtained within the electronic health record (EHR) at time of initial consultation visit.
Methods: All new patients evaluated in our clinic between 2021 to 2023 were included. Reason for visit is recorded by the registration team at scheduling. Patients complete electronic patient reported outcomes (PROs) during routine clinical care, including a 56-point review-of-systems (ROS), pain, physical function, and morning stiffness. ICD codes for inflammatory arthritis and SLE documented as a current or future encounter diagnosis, problem list, or past medical history were identified. The sample was randomly split into 80% derivation and 20% test set. Logistic regression evaluated the association of diagnosis with patient and referral data; variables with p< 0.2 in univariate were included in a multivariate model. Complete data are reported.
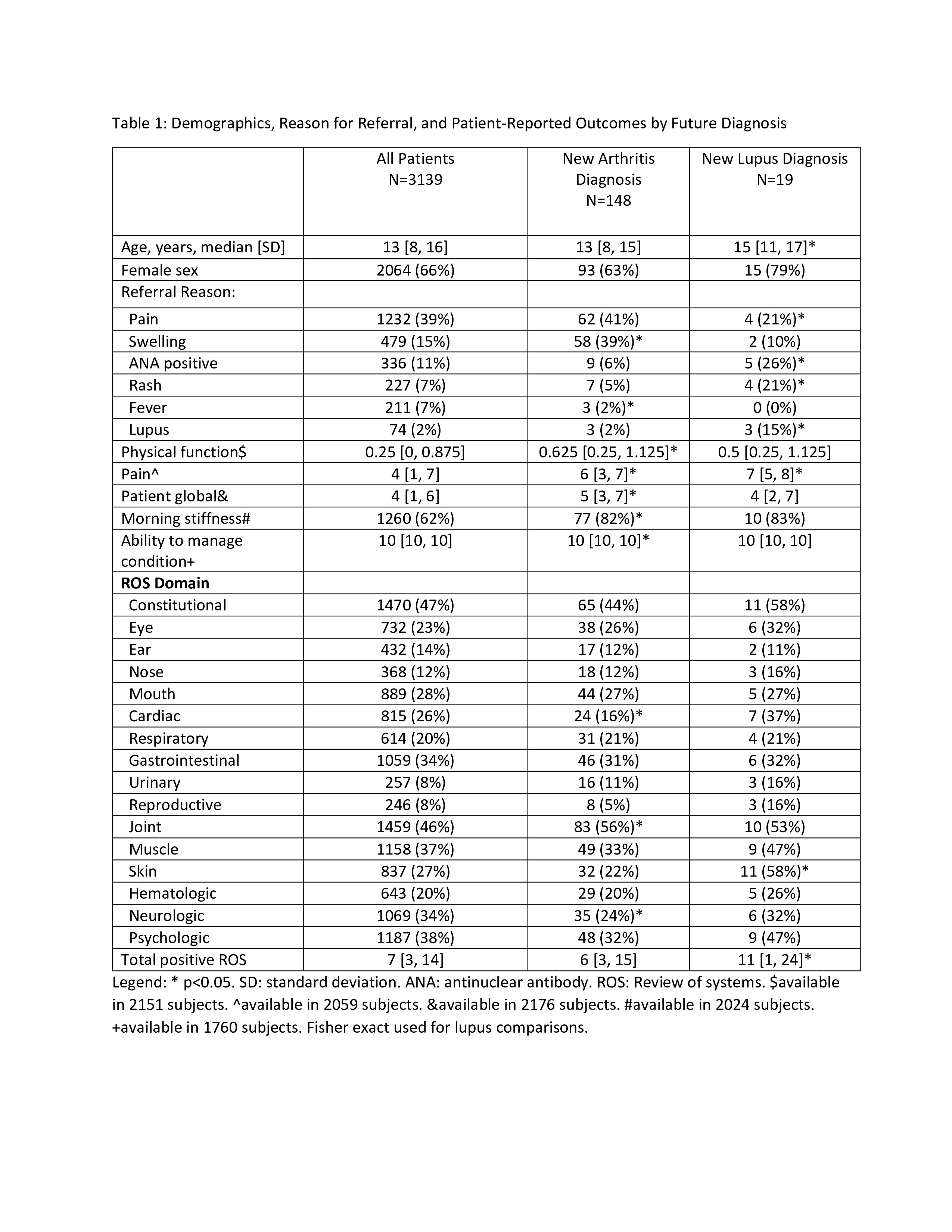
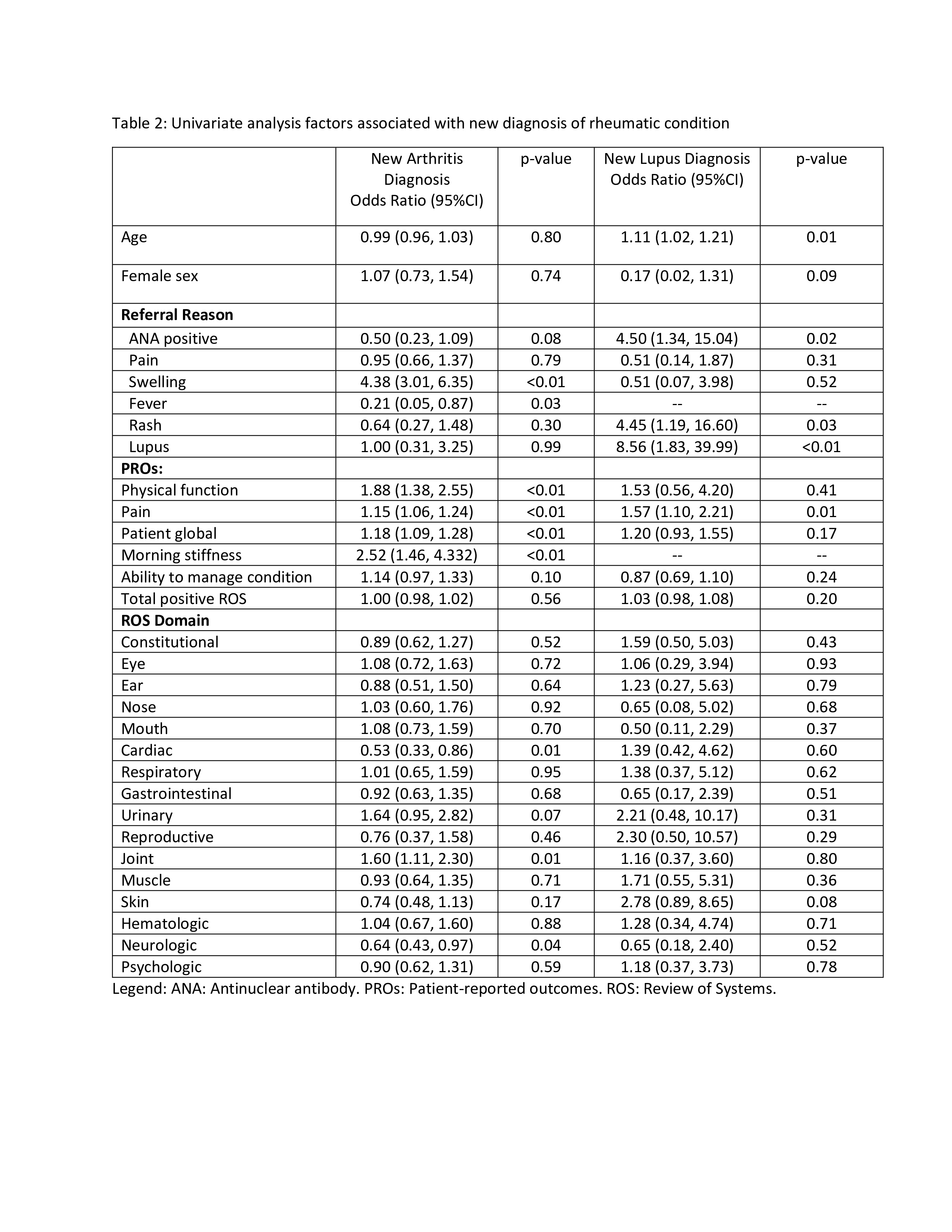
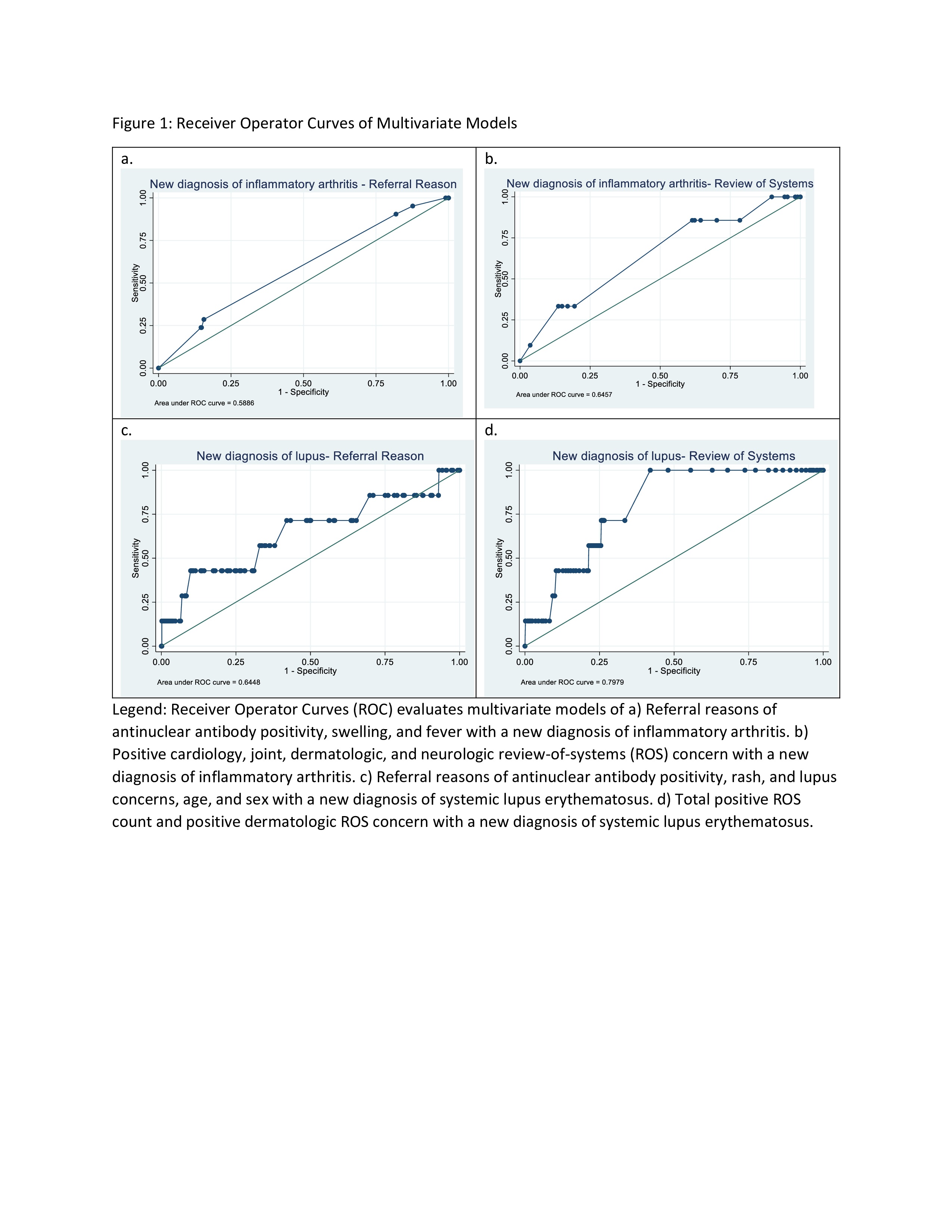
Results: There were 3139 subjects; 2064 (66%) female with a median age of 13 [IQR 8,16] (Table 1). 319 (10%) were diagnosed with arthritis with 171 (5%) already having a documented diagnosis of arthritis prior to initial consultation. There were 55 (2%) with a diagnosis of lupus during the study period with 36 (1%) diagnosed before establishing care. The median time from first visit to establishing a diagnosis of arthritis and lupus was 88 [35, 210] and 42 [17, 132] days, respectively. Common reasons for referrals included pain, swelling, and antinuclear antibody testing. There were worse physical function scores, higher pain, higher patient global score, and were more likely to report morning stiffness in those with a new diagnosis of arthritis, while higher patient-reported pain and higher positive ROS count were seen in patients with a new diagnosis of lupus. In univariate analysis, referral reasons of swelling and fever were positively and negatively associated, respectively, with a new diagnosis of arthritis while ANA positivity, rash, and lupus were positivity associated with a new diagnosis of lupus (Table 2). No referral reason variables were statistically significant in multivariate analysis. Referral data had a sensitivity of 0%, specificity of 100%, and area under the curve (AUC) of 0.59 for a new arthritis diagnosis, and a sensitivity of 0%, specificity of 100%, and AUC of 0.65 for new lupus diagnosis (Figure 1), with higher AUC when evaluating ROS data.
Conclusion: Utilization of the EHR to create a predictive algorithm for diagnosis of chronic rheumatic disease is a promising tool to address current barriers for patient care. Our data suggests that such models could be integrated into clinical referral pathways to assist with expedited access to pediatric rheumatology.
To cite this abstract in AMA style:
Lauer K, Driest K, Pratt L, Taxter A. Utilizing Electronic Health Record Pre-Consultation Data to Create a Predictive Algorithm for Diagnosis of Chronic Pediatric Rheumatic Conditions [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/utilizing-electronic-health-record-pre-consultation-data-to-create-a-predictive-algorithm-for-diagnosis-of-chronic-pediatric-rheumatic-conditions/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/utilizing-electronic-health-record-pre-consultation-data-to-create-a-predictive-algorithm-for-diagnosis-of-chronic-pediatric-rheumatic-conditions/