Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Patient care is moving from physician directed treatment to a co-design framework that focuses on creating a partnership between patients and physicians. This new framework is centered on patients’ values, with the aim of enhancing care by improving mutual understanding, goal alignment and patient-physician shared decision making (SDM). Our objective was to implement and evaluate the impact of a Rheumatoid Arthritis (RA) SDM tool, with the goal of improving SDM between RA patients and their providers.
Methods: A vital component to effectively improve outcomes in RA patients is by establishing personalized treatment plans and targets through SDM. An SDM tool (Figure 1) developed by the RISE Learning Collaborative (RISE-LC), a learning network established in March 2019 to coordinate quality improvement (QI) efforts in adult rheumatology practices across multiple centers, was introduced into our academic rheumatology clinic workflow (Figure 2) in January 2020.
We conducted a retrospective chart review of 99 patients: 50 of them with visits in September – December, prior to implementation of the SDM tool and 49 of them with a visit between January-March 2020, following tool implementation. The patients in each group categorized based on their CDAI scores: Remission: 0-2.8, Low disease activity (LDA): 2.9–10, Low-moderate disease activity (LMDA): 10.1–16, high-moderate disease activity (HMDA): 16.1–22 and high disease activity (HDA): >22. We used Minitab (Version 19.2020.1) for statistical analysis, and used two-sample t-test and two-proportion test to compare the 2 cohorts’ demographics, goals for the visit, CDAI scores, number of medications patients were on, number of associated co-morbidities and whether patients had a change in therapy.
Results: 89.9% (89/99) of the included patients were females (see Table 1). Among the patients who used the SDM tool, 65.3% used less than 2 lines to answer the question ‘what’s on my mind for today’s visit?’. Having less pain was the most common goal (65.3%) overall and this did not vary with the level of disease activity. The second most common goal was to avoid medication side effects (40.8%), which was listed more frequently for patients in LDA (47.3% or 9/19) and LMDA (50% or 6/12) groups. The patients who had a change in therapy in the non-SDM cohort were younger and had higher CDAI scores. Comparing other parameters did not reach statistical significance. See Table 1
Conclusion: Implementation of a SDM tool was feasible in our practice. Analysis of SDM tool content revealed that most patients had focused goals; less pain was the most common goal followed by having fewer medication side effects. As the disease activity increased, patients were willing to make changes to therapy. No early differences in treatment escalation were seen among those using the SDM tool, but larger studies are ongoing to assess the impact of tool implementation. Next steps also include incorporating SDM tool components into a rheumatology dashboard in our electronic health record.
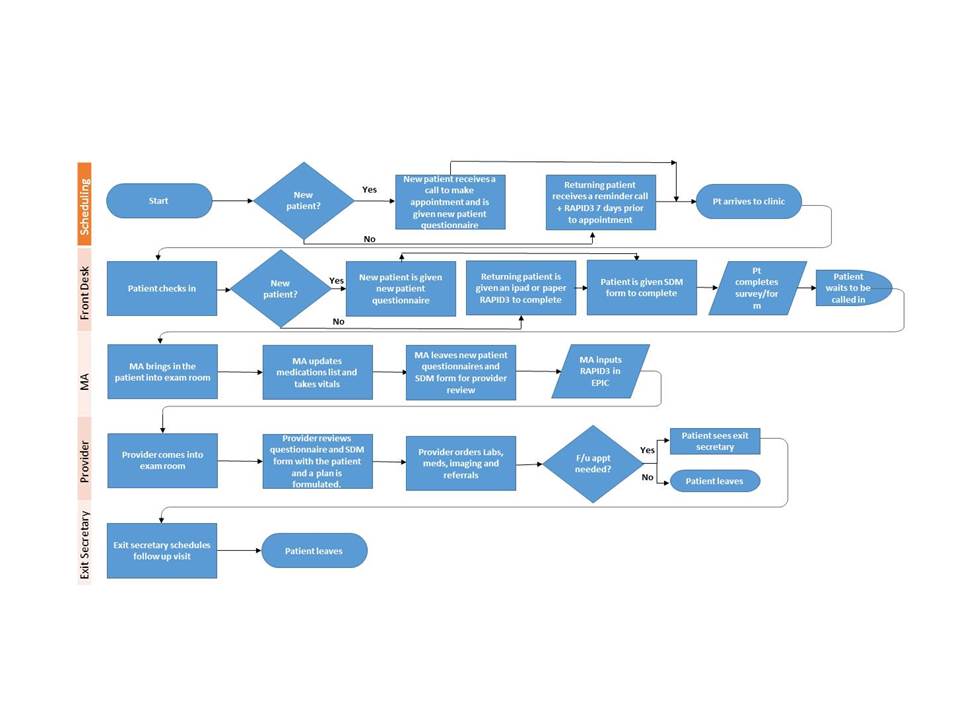 Figure 2: UT Southwestern Rheumatology Clinic Workflow
Figure 2: UT Southwestern Rheumatology Clinic Workflow
 Table 1: Comparing SDM Tool Cohort With Non-SDM Tool Cohort
Table 1: Comparing SDM Tool Cohort With Non-SDM Tool Cohort
To cite this abstract in AMA style:
Eseddi J, Bajaj P, Schmajuk G, Yazdany J, Kazi S. Using Rheumatoid Arthritis Communication Tool Developed by the RISE Learning Collaborative to Promote Shared Decision-Making [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/using-rheumatoid-arthritis-communication-tool-developed-by-the-rise-learning-collaborative-to-promote-shared-decision-making/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-rheumatoid-arthritis-communication-tool-developed-by-the-rise-learning-collaborative-to-promote-shared-decision-making/

