Session Information
Date: Monday, November 18, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Statin-induced immune-mediated necrotizing myopathy (IMNM) is a recently recognized subtype of idiopathic inflammatory myopathy (IIM). This condition is marked by the sudden onset of severe and rapidly progressing muscle weakness, accompanied by elevated serum levels of creatine kinase (CK) and of presence of myonecrosis in muscle biopsies. Despite statin discontinuation, immunosuppressive treatment remains essential to prevent muscular damage. Our study aimed to characterize a cohort of patients with IMNM with anti-3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase autoantibodies (HMGCR) and compare the clinical features and outcomes between non-relapsing (R0) and relapsing (R1) patients.
Methods: We conducted a retrospective study of patients with anti-HMGCR+ IMNM. Our cohort consisted of 48 subjects with history of lipid-lowering therapy, and with comprehensive clinical and serological data. We assessed IMACS core set disease activity measures (CSM) at baseline (t0) and 6-month (t1) follow-up (FU). An increase in CK requiring therapy modification was considered as a relapse. Statistically significant differences between groups were identified using Mann-Whitney U and Student’s t-tests. Changes over time were assessed using Friedman or Wilcoxon signed-rank tests: p values < 0,05 was considered as significant.
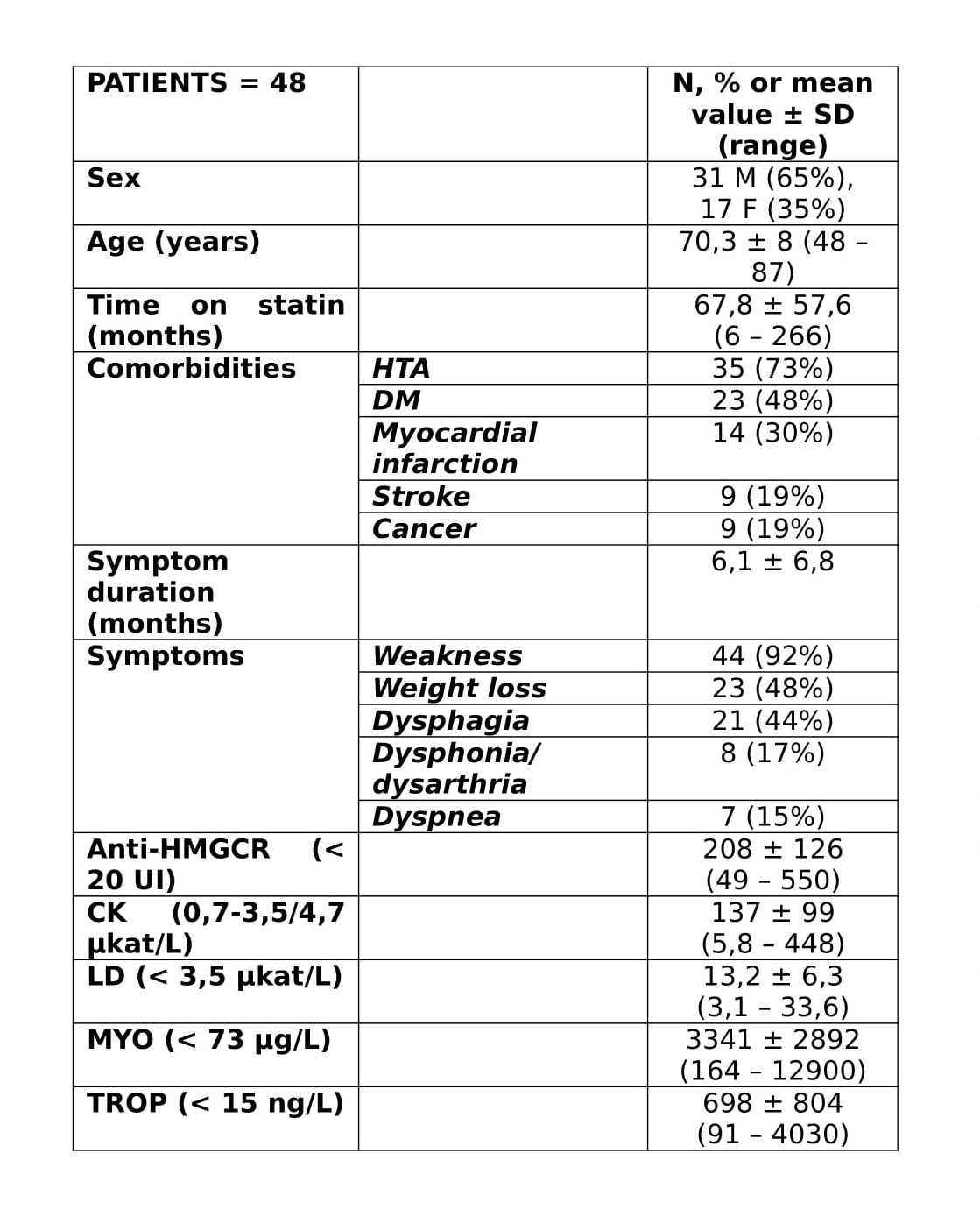
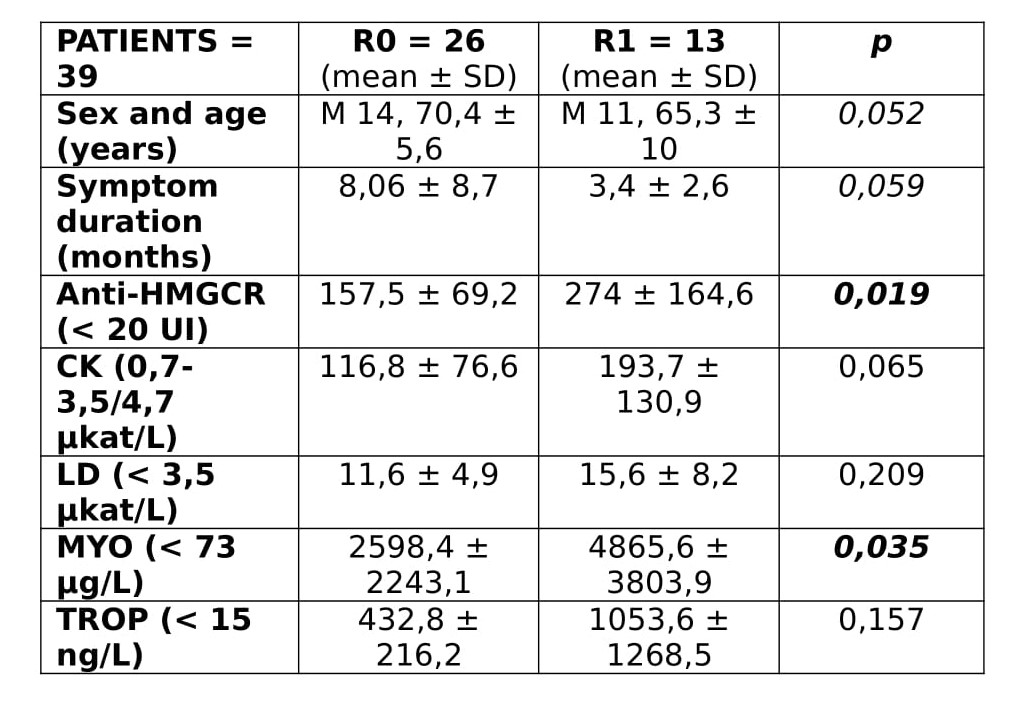
Results: Data at t0 are reported in Table 1. Anti-HMGCR autoantibody levels correlated significantly with serum levels of CK (r 0,537), myoglobin (r 0,577), troponin (r 0,710), physician global assessment (PhGA, r 0,432) and manual muscle test (MMT8, r -0,473). Symptom duration correlated with serum levels of myoglobin (r -0,570), troponin (r -0,600) and anti-HMGCR levels (r -0,359). Moreover, MMT8 correlated with serum levels of lactate dehydrogenase (r -0,587), myoglobin (r -0,535), troponin (r -0,750), PhGA (r 0,667) and CK (r -0,303). Thirty-nine patients with t1 FU were categorized based on relapse occurrence: the comparison of t0 demographic, clinical, and laboratory data is presented in Table 2. Thirteen subjects experienced at least 1 relapse: at t0, we found a statistically significant difference in anti-HMGCR levels and myoglobin. Age, symptoms duration and CK showed a trend towards significance. Interestingly, statin therapy duration and mean daily dosage did not appear to differ significantly between the groups (p=0,158, p=1) and co-administration of high-dose steroid as induction treatment did not seem to reduce relapse risk compared to IVIG-only treatment (p=0,786). During FU, both CK and anti-HMGCR antibody levels decreased significantly (p< 0,001), independently of induction therapy or relapse status, but at t1 values remained higher in R1 compared to R0 (p=0.004, p< 0,001). No differences were found in terms of total improvement score.
Conclusion: In statin-induced IMNM, relapses are more common in patients with severe disease, as demonstrated by high serum levels of anti-HMGCR antibodies and myoglobin. Additionally, higher CK, younger age, and shorter duration of symptoms might be associated with an increased risk of flares. Our findings suggest that statin dosage and therapy duration do not significantly influence the occurrence of relapses.
To cite this abstract in AMA style:
Grazzini S, Galindo-Feria A, Conticini E, Lundberg I, Dastmalchi M. Understanding Relapse Patterns in Anti-HMGCR Statin-induced IMNM: A Detailed Comparative Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/understanding-relapse-patterns-in-anti-hmgcr-statin-induced-imnm-a-detailed-comparative-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/understanding-relapse-patterns-in-anti-hmgcr-statin-induced-imnm-a-detailed-comparative-study/