Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Treatment options for pulmonary arterial hypertension (PAH) have expanded in the last two decades. However, evidence for the treatment of connective tissue disease-associated PAH (CTD-PAH) mostly depends on subgroup analysis of randomized controlled trials (RCTs). Thus, we performed a meta-analysis of the RCTs reporting outcomes for CTD-PAH.
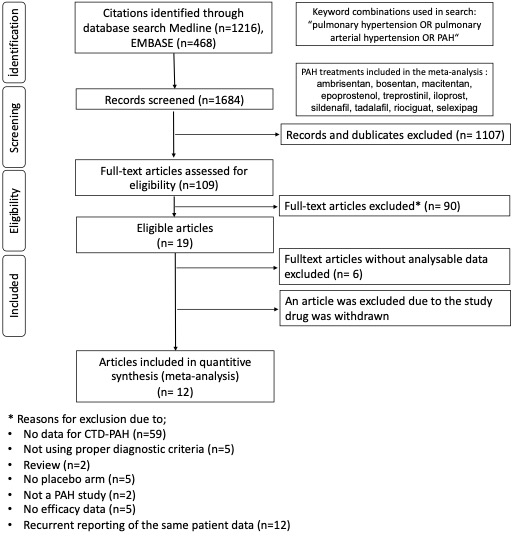
Methods: The search strategy was summarized in Figure 1. The outcomes selected for meta-analysis were functional class (FC) change, survival rates, six-minute walk distance (6-MWD), clinical worsening (CW), N-terminal prohormone BNP (NT-proBNP), pulmonary vascular resistance (PVR), mean pulmonary arterial pressure (mPAP), right atrial pressure (RAP), and cardiac index (CI). The systematic review and meta-analysis protocol was registered in PROSPERO (CRD42020153560).
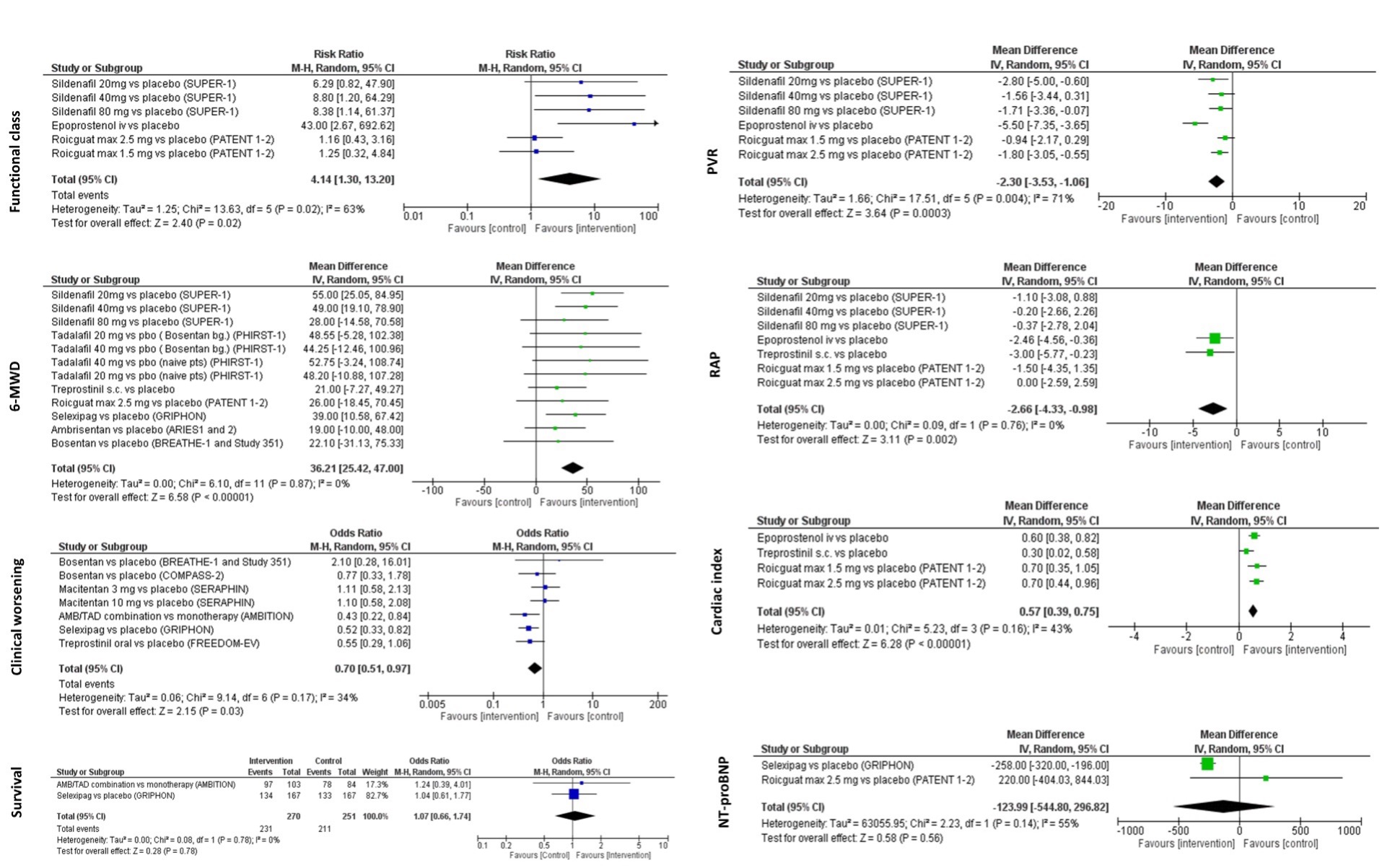
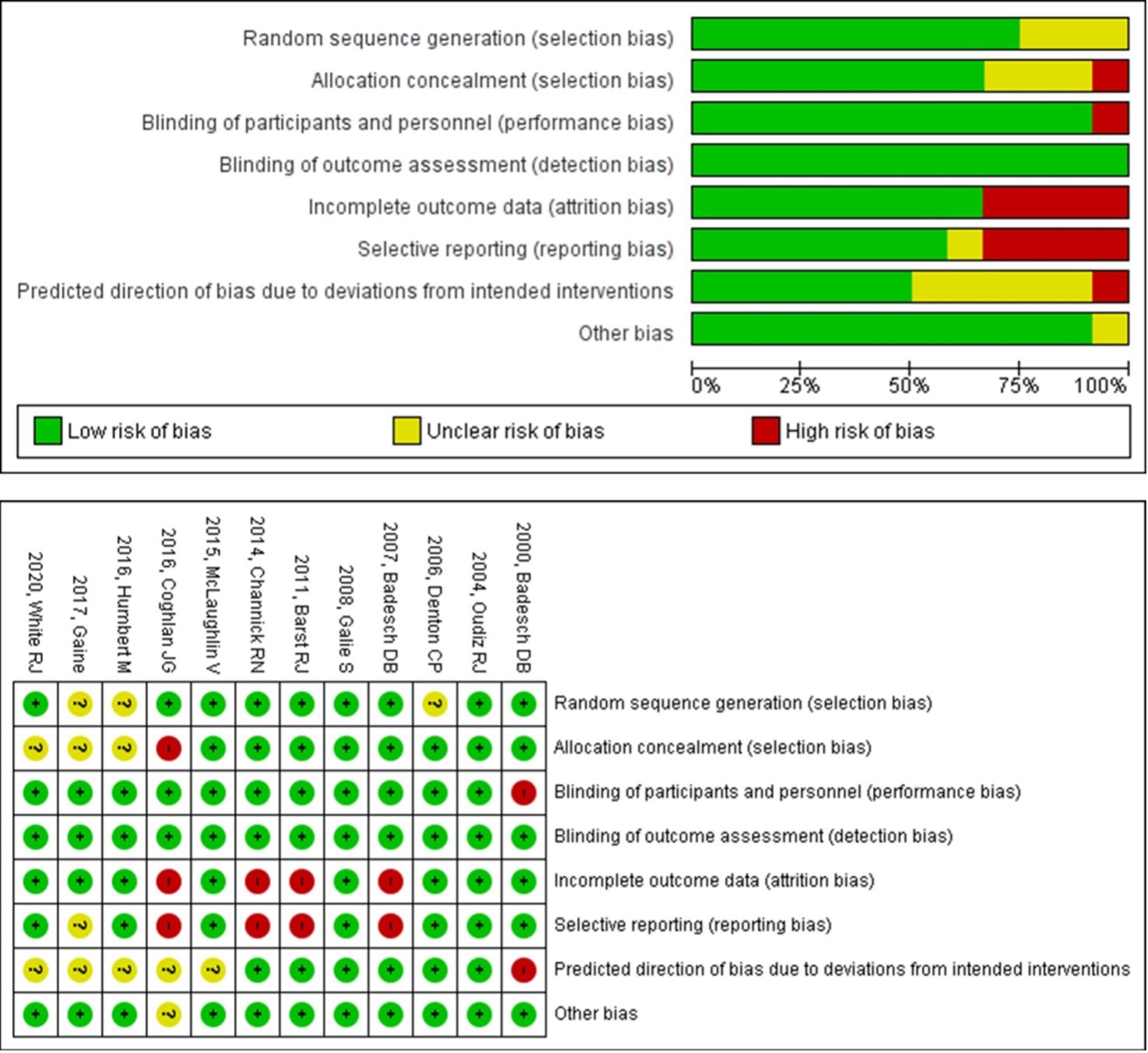
Results: PubMed and Embase searches revealed 1216 and 468 articles, respectively. After excluding the irrelevant articles and studies without available data for meta-analysis, 12 RCTs, including 1837 patients, were selected (Figure 1). The diagnoses were SSc in 59%, SLE in 20%, and other CTDs in 21%. The follow-up duration of selected trials ranged between 12 weeks to 192 weeks. The pharmacological interventions were prostacyclin analogs in 3 studies (epoprostenol in 1 study and treprostinil in 2 studies), PDE-5 inhibitors in 2 studies (sildenafil and tadalafil in one study each), ERA in 4 studies (bosentan in 2 studies, macitentan and, ambrisentan in 1 study each), riociguat in 1 study, selexipag in 1 study and, ambrisentan and tadalafil combination in 1 study. There was a significant difference between the groups in FC, 6MWD, CW, PVR, RAP, and CI, favoring the intervention arms (Figure 2.) Our analysis showed a 30% reduction in the risk of CW with PAH treatment. The reduction was higher (46%) with combination therapies. However, short-term (24-26 weeks) survival and mean serum NT-proBNP level changes were similar between groups. The RoB of the studies were summarized in Figure 3.
Conclusion: Although treatment for CTD-PAH had favorable effects on many of the clinical and hemodynamic outcomes, the effect on survival and NT-proBNP levels were not significant. This is the first meta-analysis on CTD-PAH that reported the pooled analysis of change in functional class, hemodynamic measurements (RAP, PVR, CI), and NT-proBNP, some of which have important prognostic value for PAH. Improvement in exercise capacity and reduction in risk of CW in CTD-PAH patients were less pronounced compared to idiopathic PAH (IPAH). However, changes in hemodynamic parameters in patients with CTD-PAH in our meta-analysis were similar to those in patients with IPAH in the published RCTs.
To cite this abstract in AMA style:
Erdogan M, Esatoglu S, Kilickiran Avci B, Hatemi G. Treatment of Pulmonary Arterial Hypertension in Patients with Connective Tissue Diseases: A Meta-analysis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/treatment-of-pulmonary-arterial-hypertension-in-patients-with-connective-tissue-diseases-a-meta-analysis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-of-pulmonary-arterial-hypertension-in-patients-with-connective-tissue-diseases-a-meta-analysis/