Session Information
Date: Monday, November 9, 2020
Title: Pediatric Rheumatology – Clinical II: Outcomes & Care Delivery (1983–1987)
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: To describe data-derived 2-year trajectories of disease activity in patients with recently diagnosed juvenile idiopathic arthritis (JIA) as measured by the clinical Juvenile Arthritis Disease Activity Score measured in 10 joints (cJADAS10), and to identify key baseline characteristics associated with disease trajectories.
Methods: The Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry includes a large cohort of children with JIA with clinical and medication data. JIA patients eligible for this study were enrolled between April 15, 2016 and December 6, 2019, within 3 months of JIA diagnosis, had at least 2 follow-up (FU) visits with cJADAS10 scores, and had 24 months of FU. Latent trajectory analysis of cJADAS10 using maximum likelihood estimation technique was performed. Model of best fit was selected by a combination of Bayesian information criterion (BIC), posterior probabilities, and clinical judgement. Select pairwise comparisons of baseline characteristics by trajectory were performed.
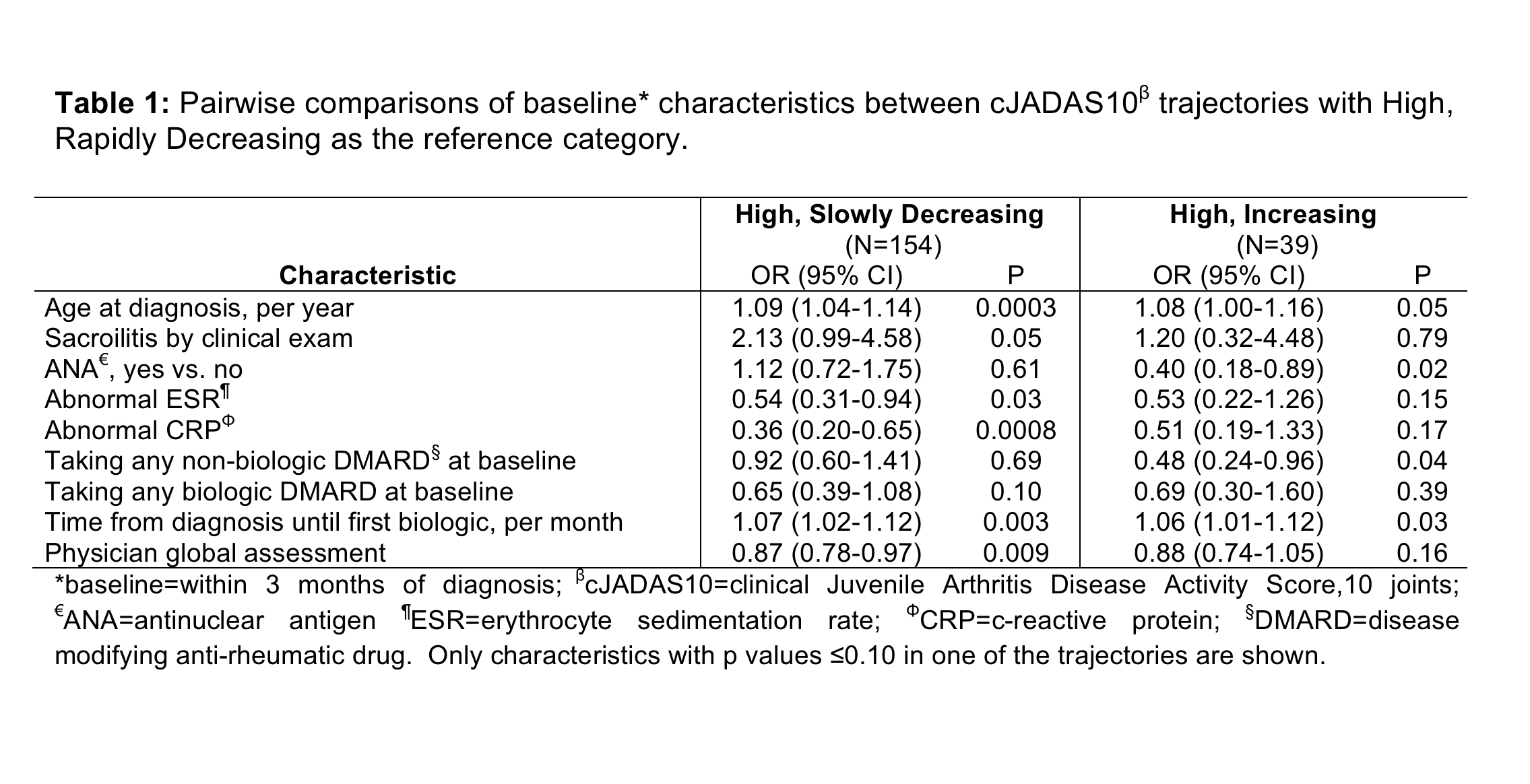
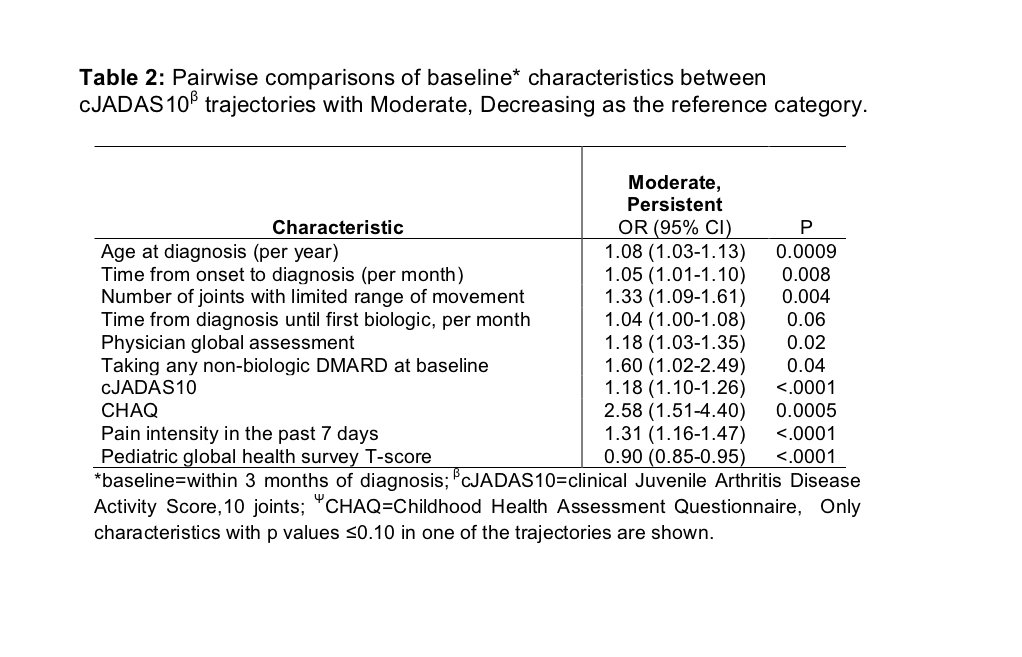
Results: There were 8,736 JIA patients in the Registry; 746 met study selection criteria. Clinician assigned JIA categories were: 32.6% rheumatoid factor (RF) negative polyarticular, 26.0% oligoarticular, 13% enthesitis related arthritis, 10.6% RF positive polyarticular, 8.7% systemic, 7.0% psoriatic, and 2.1% undifferentiated. Figure 1 shows the model of best fit, which identified 5 disease trajectories: High, Rapidly Decreasing (HRD) (n=199, 26.7%); High, Slowly Decreasing (HSD) (n=154, 20.6%); High, Increasing (HI) (n=39, 5.2%); Moderate, Persistent (MP) (n=218, 29.2%); and Moderate, Decreasing (MD) (n=136, 18.2%). When compared to the HRD trajectory, patients with a HSD trajectory were more likely to be older, have normal erythrocyte sedimentation rate and c-reactive protein, longer time from diagnosis to first biologic, and a lower baseline physician global assessment (PGA). Those with a HI trajectory were more likely to be ANA negative, have a longer time from diagnosis to first biologic, and less likely to be taking a non-biologic disease modifying anti-rheumatic drug (DMARD) at baseline (Table 1). Patients starting with moderate cJADAS10 scores with MP trajectory were more likely to be older, have a longer time from onset to diagnosis, more joints with restricted range, taking a non-biologic DMARD at baseline, have higher PGA, cJADAS10, CHAQ, and pain intensity, and lower pediatric global health survey scores at baseline (Table 2).
Conclusion: This study identified 5 distinct data derived trajectories of JIA disease activity. Baseline variables associated with concerning trajectories are described, and could assist with targeting patients for more aggressive intervention shortly after diagnosis.
 Figure 1. Trajectories of cJADAS10 with 95% CIs in patients with juvenile idiopathic arthritis (n=746)
Figure 1. Trajectories of cJADAS10 with 95% CIs in patients with juvenile idiopathic arthritis (n=746)
To cite this abstract in AMA style:
Shiff N, Shrader P, Correll C, Dennos A, Phillips T, Beukelman T. Trajectories of Disease Activity in Patients with Newly Diagnosed Juvenile Idiopathic Arthritis in the Childhood Arthritis and Rheumatology Research Alliance Registry [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/trajectories-of-disease-activity-in-patients-with-newly-diagnosed-juvenile-idiopathic-arthritis-in-the-childhood-arthritis-and-rheumatology-research-alliance-registry/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/trajectories-of-disease-activity-in-patients-with-newly-diagnosed-juvenile-idiopathic-arthritis-in-the-childhood-arthritis-and-rheumatology-research-alliance-registry/