Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Childhood-onset systemic sclerosis (SSc) is a rare but potentially life-threatening autoimmune condition with features including immune, fibrotic, and vascular manifestations affecting the skin and other internal organs, such as the cardiac, pulmonary, and gastrointestinal systems. Compared to adults with SSc, a greater proportion of pediatric SSc patients have overlap syndrome. Information about pediatric SSc overlap syndrome is lacking given the overall rarity of this condition and there is a notable gap in knowledge. We report on 4 patients diagnosed with SSc overlap syndrome from a single large pediatric center.
Methods: This project was conducted under IRB approval from Baylor College of Medicine. A retrospective chart review of patients who fulfilled the 2007 PRES/ACR/EULAR juvenile SSc provisional classification criteria between 2000 to 2022 was conducted. Patients with SSc overlap syndrome who also fulfilled the 2017 EULAR/ACR classification criteria for juvenile dermatomyositis (JDM) or 2012 SLICC criteria for lupus were identified. Information, including demographics, clinical features, diagnostic findings, and outcomes were collected.
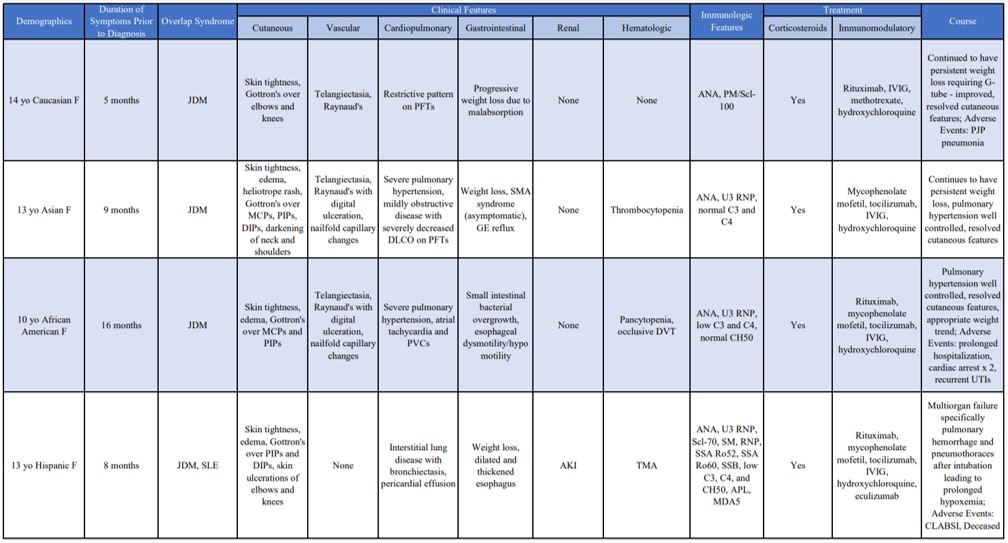
Results: During the inclusion period, a total of 21 patients were diagnosed with SSc and 4 (19%) were classified as overlap syndrome. All had features of JDM with one patient having additional lupus features. All patients were female with a mean age at diagnosis of 12.5 years (range 10 – 14 years). The average time between symptom onset and time of diagnosis was 9.5 months (5 – 16 months). JDM features included cutaneous Gottrons rash and myositis based on clinical exam, labs, and/or imaging, and lupus features included hematologic manifestations and serositis. All patients had positive antinuclear antibodies (ANA), while 3 of 4 had a positive U3-RNP antibody. Two patients had hypocomplementemia. Renal disease was not seen in the patient with lupus features, and no patient developed scleroderma renal crisis. All patients received systemic corticosteroids and additional immunomodulatory therapies including rituximab, IVIG, and mycophenolate mofetil. Improvement of the SSc cutaneous features and resolution of the JDM skin changes were noted in all patients. All patients had either recurrences or progression of gastrointestinal and cardiopulmonary manifestations throughout their course despite treatment. Adverse events included prolonged hospitalizations, infections, and death (Table 1).
Conclusion: SSc overlap syndrome is a rare, difficult disease associated with significant morbidity and even mortality in pediatric patients. Cutaneous manifestations improved with multimodal pharmacotherapy while cardiopulmonary and gastrointestinal involvement continued to be a source of morbidity despite treatment. Renal manifestations were not seen throughout the clinical course. Treatment with systemic corticosteroids was well tolerated and choice of immunomodulatory agents was tailored to both the scleroderma and overlapping inflammatory disorder. Further studies need to be done to determine if there are differences in clinical course and prognosis between juvenile SSc and SSc overlap syndrome.
To cite this abstract in AMA style:
Nguyen J, Gillispie-Taylor M, Muscal E, Deguzman M. Systemic Sclerosis Overlap Syndrome: A Case Series from a Single Large Pediatric Center [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/systemic-sclerosis-overlap-syndrome-a-case-series-from-a-single-large-pediatric-center/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/systemic-sclerosis-overlap-syndrome-a-case-series-from-a-single-large-pediatric-center/