Session Information
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
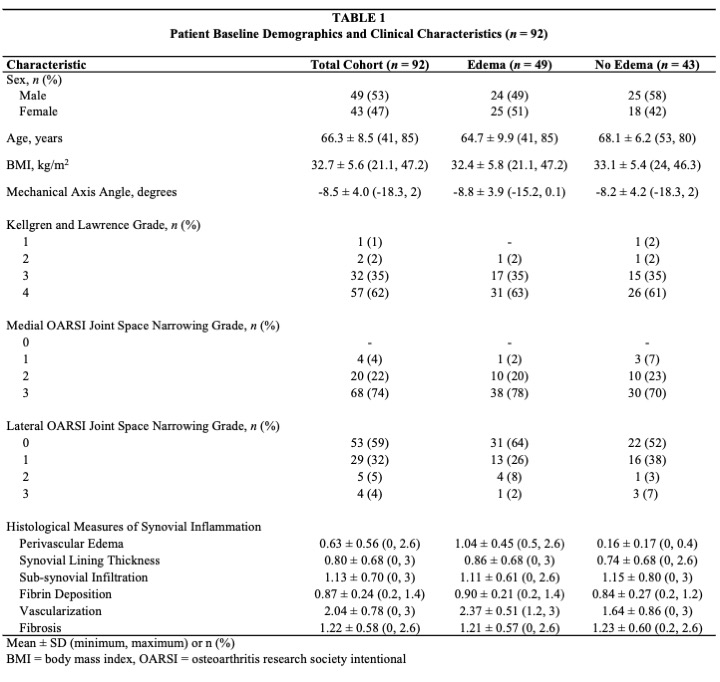
Background/Purpose: Synovial inflammation and aberrant joint loads are independent risk factors for knee osteoarthritis (OA) incidence and progression. Perivascular edema, the accumulation of fluid around synovial blood vessels (Figure 1), is an important component of synovial inflammation in OA. Altered joint loading is hypothesized to contribute to synovial inflammation in OA and may provide sufficient physiological stress to induce perivascular edema. Our objective was to investigate the association between synovial perivascular edema and surrogate measures of knee load during walking in patients with knee OA and medial compartment joint space narrowing.
Methods: Patients undergoing total knee arthroplasty or high tibial osteotomy for symptomatic, radiographic knee OA based on the American College of Rheumatology Classification Criteria, and neutral to varus alignment participated in this cross-sectional study. All participants underwent 3D gait analysis before surgery. Synovial biopsies were obtained intra-operatively for histopathological assessment of perivascular edema (presence/absence). We investigated the association between external knee moments (sagittal, frontal, and transverse planes) and the presence of synovial perivascular edema using a series of multivariate linear regression and polynomial mixed-effects regression models, while adjusting for age, sex, BMI, and gait speed.
Results: Our cohort was composed of 92 patients with complete gait and histopathological data (Table 1). The presence of perivascular edema was associated with lower peak knee flexion moment (β= -7.72 Nm [95%CI -14.18, -1.27]) and greater peak knee extension moment (β= -8.08 Nm [95%CI -15.26, -0.89]). Mixed-effects polynomial regression identified that patients with edema demonstrated higher knee adduction moments between 16-74% of stance (Figure 2A), and lower knee flexion moments from 15-92% of stance (Figure 2B). The largest differences in knee moments during walking between patients with vs. without perivascular edema occurred at 33% of stance for knee adduction (β= 6.87 Nm [95%CI 3.02, 10.72]), and 60% of stance for knee flexion (β = -10.80 [95%CI -16.20, -5.40]).
Conclusion: Although causal inference is not possible, the association of synovial perivascular edema with increased gait-based proxy measures of knee loading throughout all phases of stance supports the hypothesis that abnormal joint biomechanics contribute to synovial inflammation in knee OA. Future research is needed to identify direct or indirect mechanisms linking altered joint loading to the development of synovial perivascular edema.
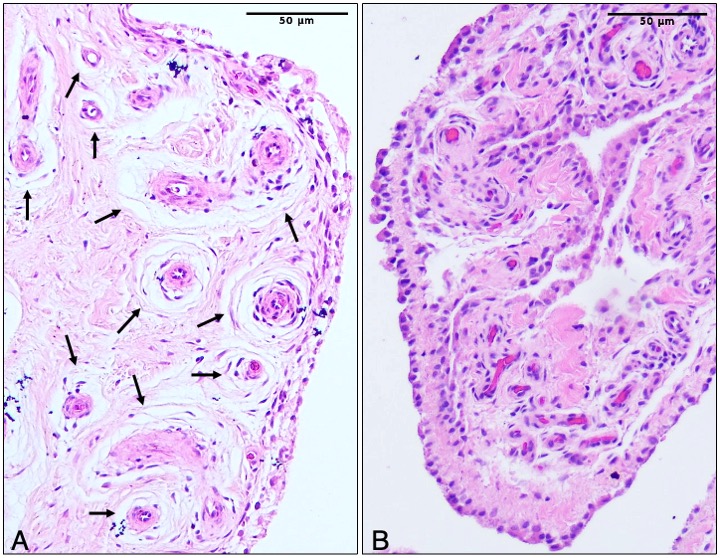 Figure 1. Representative histological images of synovial perivascular edema. Histological evidence of the presence (A) and absence (B) of perivascular edema in synovial biopsies acquired from patients with knee OA. Vessels with perivascular edema are indicated with black arrows.
Figure 1. Representative histological images of synovial perivascular edema. Histological evidence of the presence (A) and absence (B) of perivascular edema in synovial biopsies acquired from patients with knee OA. Vessels with perivascular edema are indicated with black arrows.
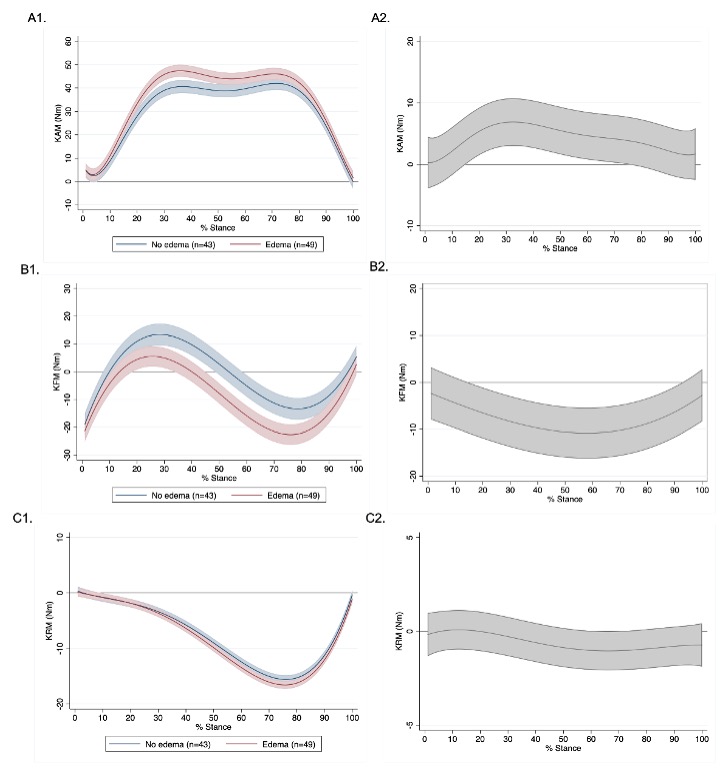 Figure 2. Marginal effects and contrasts for external knee moments over 100% of stance phase in patients with perivascular edema and no perivascular edema. Marginal effect estimates (± 95% CIs) for external knee moments by group are shown in left panels (A1-C1) and marginal contrasts (± 95% CIs) for external knee moments between patients with perivascular edema (n=49) and no perivascular edema (n=43) are shown in the right panels (A2-C2). Separate graphs for A) knee adduction moment (KAM), B) knee flexion-extension moment (KFM), and C) knee external-internal rotation moment (KRM). No perivascular edema is represented in blue and perivascular edema is represented in red. No perivascular edema is the reference group for the marginal contrasts (right panels: A2-C2); therefore, along stance phase, where the 95% CIs no longer includes 0, indicates a significant difference between groups.
Figure 2. Marginal effects and contrasts for external knee moments over 100% of stance phase in patients with perivascular edema and no perivascular edema. Marginal effect estimates (± 95% CIs) for external knee moments by group are shown in left panels (A1-C1) and marginal contrasts (± 95% CIs) for external knee moments between patients with perivascular edema (n=49) and no perivascular edema (n=43) are shown in the right panels (A2-C2). Separate graphs for A) knee adduction moment (KAM), B) knee flexion-extension moment (KFM), and C) knee external-internal rotation moment (KRM). No perivascular edema is represented in blue and perivascular edema is represented in red. No perivascular edema is the reference group for the marginal contrasts (right panels: A2-C2); therefore, along stance phase, where the 95% CIs no longer includes 0, indicates a significant difference between groups.
To cite this abstract in AMA style:
Carter M, Philpott H, Birmingham T, Pinto R, Primeau C, Giffin J, Lanting B, Appleton T. Synovial Perivascular Edema Is Associated with Altered Knee Loading Patterns During Gait in Patients with Medial Compartment-Dominant Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/synovial-perivascular-edema-is-associated-with-altered-knee-loading-patterns-during-gait-in-patients-with-medial-compartment-dominant-knee-osteoarthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/synovial-perivascular-edema-is-associated-with-altered-knee-loading-patterns-during-gait-in-patients-with-medial-compartment-dominant-knee-osteoarthritis/