Session Information
Date: Sunday, October 26, 2025
Title: (0430–0469) Rheumatoid Arthritis – Diagnosis, Manifestations, and Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Synovial tissue pathotype may indicate treatment response in RA, but synovial biopsies are not widely available. Synovial fluid (SF) is a promising surrogate. We sought to identify SF features that reflect histopathological and clinical characteristics in RA.
Methods: SF and synovial tissue were prospectively collected from patients meeting RA criteria undergoing total knee replacement. SF white blood cell (WBC) count and differentials were analyzed in the clinical laboratory. Patients were stratified into three groups by medication history: “biologic naïve,” “on biologic” and “refractory.” Synovial Lymphocytic Inflammation (SLI) was graded from low (0-2) to high (3) inflammation by a board-certified pathologist. Descriptive statistics, correlations, ROC curve, and multivariate regressions were used to assess associations with SF cell counts. Separately, a retrospective review of the electronic medical record (EMR) extracted SF parameters, clinical characteristics, and patient reported outcome measures (PROMs) from patients who underwent joint aspirations between 2017 and 2023. Infections, gout, and CPPD were defined by positive cultures or appropriate crystal identification; other diagnoses were determined using ICD-10 codes. PROMs included the Multidimensional Health Assessment Questionnaire (MDHAQ), and Routine Assessment of Patient Index Data 3 (RAPID3).
Results: In 64 RA patients with paired synovial tissue histology and SF cell counts, mean SF WBC was 5,661 cells/µL, and mean CDAI was 17.9 (Table 1). 29 (45%) had high SLI, which correlated positively with SF WBC (Figure 1A). Patients in the high SLI group had higher mean CRP (2.4 vs. 0.6, p< 0.0001), swollen joint count (5.7 vs. 3.8, p=0.021), CCP positivity (86% vs 63%, p=0.035), and DAS28-CRP (4.2 vs 3.3, p=0.014) compared to patients in the low SLI group. There were no differences in disease activity or SLI between medication groups. SF WBC ≥ 1400 cells/µL was sensitive (0.86) and specific (0.91) for high SLI (AUC 0.91) (Figure 1B). The proportion of aspirations with WBC ≥ 1400 cells/µL varied by diagnosis in the retrospective chart review (Figure 1C). Of 2,171 aspirations, 823 were from RA patients, of whom 492 (60%) had WBC ≥ 1400 cells/µL. Septic arthritis and OA had the highest and lowest proportion of WBC ≥ 1400 cells/µL, respectively. Compared to those with WBC < 1400 cells/µL, RA patients with WBC ≥ 1400 cells/µL had higher mean ESR (38.7 vs 23.0, p< 0.0001), CRP (10.9 vs 6.7, p=0.0008), and SF PMN% (61.1 vs. 17.8, p< 0.0001) (Table 2). RA patients with WBC ≥ 1400 cells/µL had significantly lower mean RAPID3 scores (11.9 vs 14.1, p=0.0213) compared to those with WBC < 1400 cells/µL. Mean MDHAQ scores did not differ significantly between the two WBC groups.
Conclusion: SF WBC is sensitive and specific for differentiating high and low SLI in RA. SF WBC ≥ 1400 cells/µL was associated with higher measures of systemic inflammation when collected intra-operatively and during routine aspiration but not with composite measures of disease activity or PROMs, suggesting that the SF WBC count provides distinct information that may be useful in selecting appropriate anti-inflammatory targeted therapy.
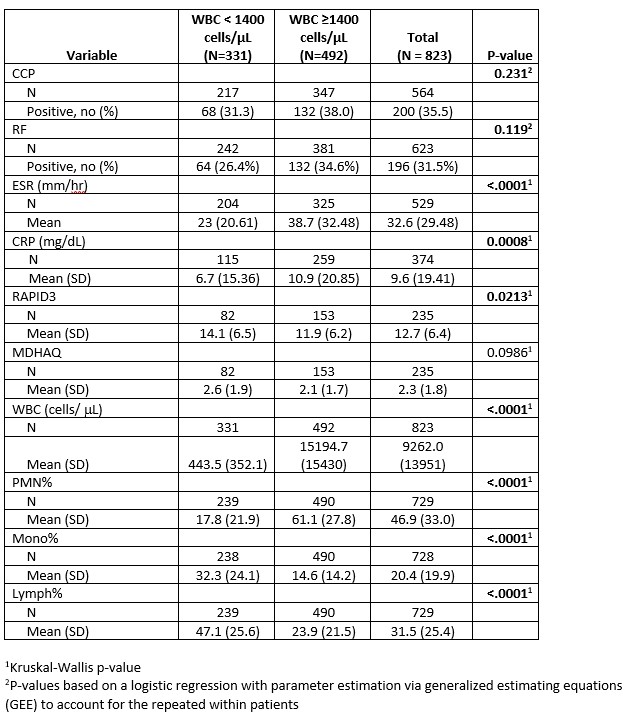 Table 1. Demographic and clinical characteristics stratified by low (0-2)^1 and high (3)^2 synovial lymphocytic inflammation (SLI) for RA patients with paired synovial tissue histology and SF data.
Table 1. Demographic and clinical characteristics stratified by low (0-2)^1 and high (3)^2 synovial lymphocytic inflammation (SLI) for RA patients with paired synovial tissue histology and SF data.
.jpg) Figure 1. Synovial fluid cellularity predicts synovial tissue inflammation in RA and varies by diagnosis. 1A) Scatterplot depicting increasing synovial tissue lymphocytic inflammation (0-3B) vs. synovial fluid white blood cell (WBC) count (cells/µL). B = SLI 3-band. Kruskal-Wallis chi-square = 36.9, df = 4, p < 0.001. 1B) Synovial fluid cellularity predicts the degree of tissue inflammation. Receiver Operator Curve using synovial fluid threshold ≥ 1400 WBC/µL to classify synovial tissue with grade 3 SLI. 1C) Fraction of aspirations associated with each diagnosis with > 1400 WBC/µL.
Figure 1. Synovial fluid cellularity predicts synovial tissue inflammation in RA and varies by diagnosis. 1A) Scatterplot depicting increasing synovial tissue lymphocytic inflammation (0-3B) vs. synovial fluid white blood cell (WBC) count (cells/µL). B = SLI 3-band. Kruskal-Wallis chi-square = 36.9, df = 4, p < 0.001. 1B) Synovial fluid cellularity predicts the degree of tissue inflammation. Receiver Operator Curve using synovial fluid threshold ≥ 1400 WBC/µL to classify synovial tissue with grade 3 SLI. 1C) Fraction of aspirations associated with each diagnosis with > 1400 WBC/µL.
.jpg) Table 2. Comparison of clinical characteristics and patient reported outcome measures (PROMs) for Synovial Fluid (SF) aspirations of RA patients stratified by the SF white blood cell (WBC) count.
Table 2. Comparison of clinical characteristics and patient reported outcome measures (PROMs) for Synovial Fluid (SF) aspirations of RA patients stratified by the SF white blood cell (WBC) count.
To cite this abstract in AMA style:
Cushing S, Goodman S, Parides M, Abdul-Rehman H, Ramirez D, DiCarlo E, Carandang K, Davis R, Blank R, Donlin L, Jonsson A, Lakhanpal A, Mehta B, Orange D, smith M. Synovial fluid is a robust biomarker of synovial tissue inflammation in rheumatoid arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/synovial-fluid-is-a-robust-biomarker-of-synovial-tissue-inflammation-in-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/synovial-fluid-is-a-robust-biomarker-of-synovial-tissue-inflammation-in-rheumatoid-arthritis/
