Session Information
Date: Monday, November 8, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster II (1364–1390)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Based on the argument that symptoms-define-disease, physicians commonly apply the terms pre-clinical or sub-clinical disease to describe patients with disease-related findings, but no accompanying symptoms. For patients with connective tissue disease associated interstitial lung disease (CTD-ILD), the term sub-clinical applies frequently to patients with mild ILD changes on HRCT, within normal range functional capacity and no respiratory symptoms. Previous work in systemic sclerosis (SSc)-ILD did however show that patients with even minor extent of ILD at baseline often progressed and had increased mortality risk; indicating that it is not appropriate to define these patients as “subclinical”. The objective of this study was to to identify the prevalence of subclinical ILD across CTD diagnoses, and assess the rate of progression of lung fibrosis compared to CTD without ILD and with clinical ILD.
Methods: All CTD patients, including SSc, anti-syntethase syndrome (ASS) and mixed connective tissue disease (MCTD) from the Oslo University Hospital diagnosed before 2015 assessed for the presence of ILD by HRCT were included. 2015 was chosen to secure an observation time of at least 5 years from ILD diagnosis to study end on 01.01.2021 or time of death. All patients fulfilled the respective CTD classification criteria. Subclinical ILD was defined as an ILD extent < 5% by semi-quantitative assessment at baseline HRCT, preserved lung function with a forced vital capacity (FVC) >80%predicted and no respiratory symptoms. Clinical ILD was defined as >5% extent of ILD or < 5% extent of ILD on HRCT with respiratory symtoms or FVC< 80%. The outcome was progression of lung fibrosis assessed on HRCT at follow up. Vital status was available in all patients and mortality assessed. Descriptive statistical analyses were conducted and time to progressive event determined by Kaplan-Meier estimates.
Results: We identified 525 CTD patients, including 296 SSc, 135 MCTD and 94 ASS patients assessed for ILD. Of these, 227 (43%) had no ILD, 67 (13%) subclinical and 231 (44%) clinical ILD (Table). Of the 67 subclinical ILD patients, 45 (15%) had SSc, 13 (10%) MCTD and 9 (10%) ASS. Over a median time of 4.5 years between baseline and follow up HRCT, 95/395 (24%) showed lung fibrosis progression, including 72 (26%) SSc and 23 (19%) MCTD patients. Disease progression was frequently present in both subclinical ILD (38%) and clinical ILD (51%) patients (Figure). Age, gender, underlying CTD and baseline lung function were not predictive for lung fibrosis progression. The events were too low for multivariable regression analyses. After a median observational period of 12 years, 153 (29%) of the patients died. The 1-, 5- and 10-year survival rates in no ILD, subclinical and clinical ILD were 97%/97%/99%, 88%/91%/82% and 82%/85%/68% (p< 0.001), respectively.
Conclusion: Subclinical ILD is frequently present across CTDs and progresses over time in a substantial subgroup of patients, comparable to patients with clinical ILD. Our findings question the terms sub- and preclinical ILD, which may potentially lead to to a suboptimal “watchful waiting management strategy”.
 Table1: Clinical characteristics, demographics and outcome of CTD without ILD, and with subclinical and clinical ILD
Table1: Clinical characteristics, demographics and outcome of CTD without ILD, and with subclinical and clinical ILD
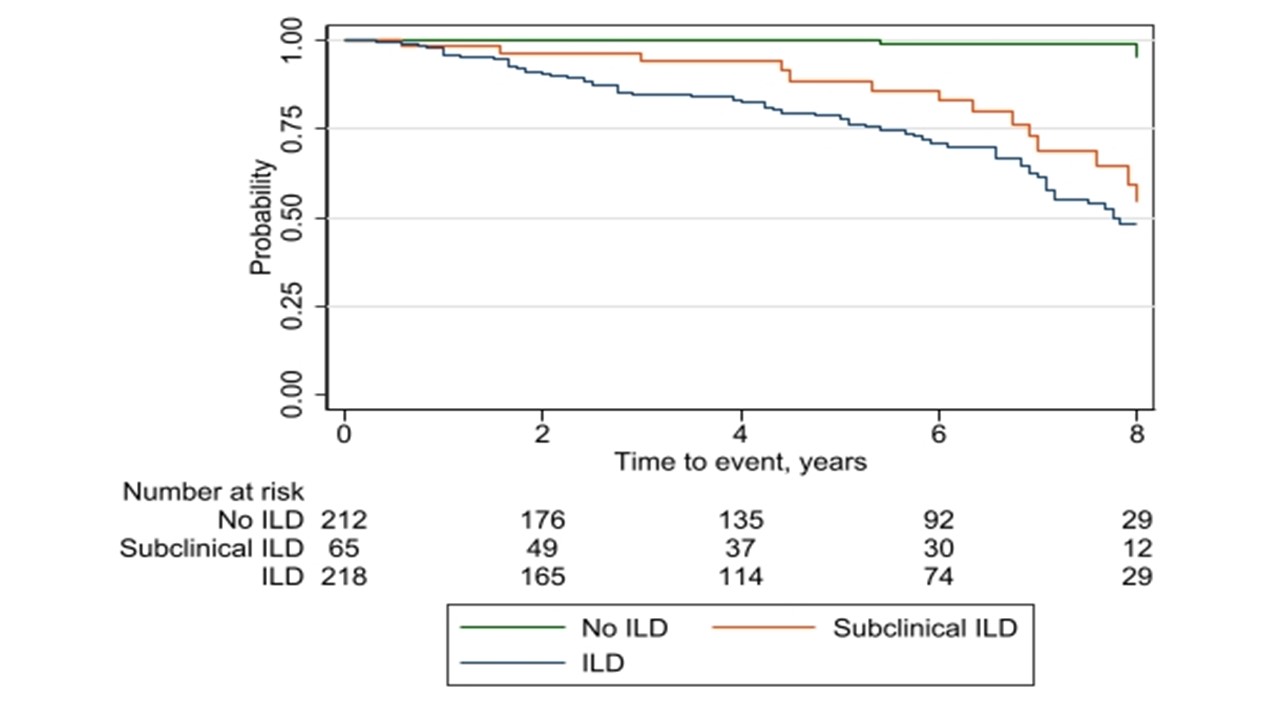 Figur 1: Time to progressive event
Figur 1: Time to progressive event
To cite this abstract in AMA style:
Hoffmann-Vold A, Andersson H, Reiseter S, Fretheim H, Barua I, Garen T, Midtvedt , Gunnarsson R, Durheim M, AAløkken T, Molberg. Subclinical ILD Is Frequent and Progresses Across Different Connective Tissue Diseases [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/subclinical-ild-is-frequent-and-progresses-across-different-connective-tissue-diseases/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subclinical-ild-is-frequent-and-progresses-across-different-connective-tissue-diseases/
