Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Salivary gland ultrasound (SGUS) abnormalities have been increasingly recognized as possible biomarkers for Sjögren’s Syndrome (SS) phenotypic stratification. However, to date few studies have investigated the association between SGUS and anti-Ro/SSA serological status (i.e. seronegative, isolated anti-Ro52, double positive anti-Ro52/Ro60 and isolated anti-Ro60). Our aims were to explore the association between SGUS and anti-Ro/SSA sub-specificities and to determine whether SGUS combined with anti-SSA status may drive cluster phenotypes in SS.
Methods: Consecutive patients newly diagnosed with pSS (ACR 2016) were included in the study from January 2017. All patients underwent anti-Ro/SSA detection, salivary flow measurement (UWS) and ocular tests. Patients’ clinical, biological and salivary gland ultrasonographic (SGUS) features were prospectively collected. Extra-glandular manifestations were assessed according to the ESSDAI. PROs were collected (ESSPRI, VAS ocular, oral and global dryness, VAS fatigue, VAS pain, OSDI and OHIP). For each of the MSGs specimen number of foci, focus score (FS) and ectopic lymphoid structures (ELS) were assessed. We did cluster two step analysis using anti-Ro/SSA status and SGUS≥2 to identify subgroups in our cohort. Clinical, biological and histological data were compared among the subgroups.
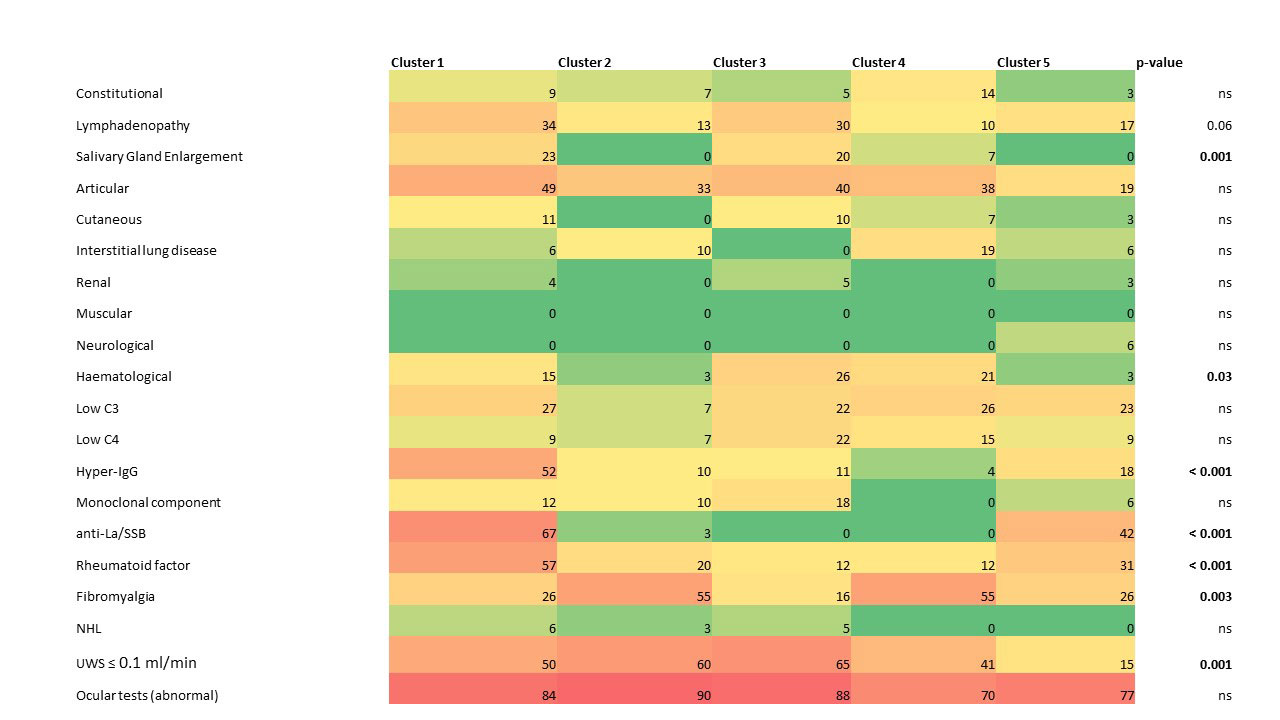
Results: We included 200 pSS patients (181 F:19 M; mean age 55.9±12.9 yrs; 157/200 (78.5%) anti-Ro/SSA+). We identified 5 subgroups in the cohort (FIG1.): cluster 1 with anti-Ro52+/Ro60+ and SGUS≥2, cluster 2 with predominant anti-Ro52-/antiRo60- and SGUS< 2, cluster 3 with predominant isolated anti-Ro52 and SGUS≥2, cluster 4 with isolated anti-Ro52 and SGUS< 2 and cluster 5 with anti-Ro52+/Ro60+ (70%) and SGUS< 2. The 5 clusters did not differ in demographic features. Patients in cluster 1 presented the highest number of foci, FS and ELS; however, in pair-wise comparisons histology differences were statistically significant only when tested against cluster 4 and cluster 2. A similar trend was observed for B cell hyperactivity biomarkers (i.e hypergammaglobulinemia, lymphadenopathy, SSB) and for the ESSDAI glandular and haematological domains. Cluster 1 and 5 particularly differed in total ESSDAI score and UWS that was still preserved in the latter. Cluster 3 presented a significantly higher number of Foci and FS than cluster 4. Differences among the clusters are summarized in the heatmap (FIG 1).
Conclusion: SGUS identified subclinical sialadenitis in pSS patients, thus allowing to recognize distinct clinical subsets with more severe tissue inflammation, glandular dysfunction, and B-cell hyperactivity, ultimately improving serological-based stratification.
To cite this abstract in AMA style:
Fonzetti S, Ferro F, La Rocca G, Fulvio G, Navarro García I, Governato G, Donati V, Mosca M, Baldini C. Salivary Gland Ultrasound May Lead to a More Accurate Stratification of Patients with the Same Serological Profile in Sjögren’s Syndrome: Towards a Personalized Approach [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/salivary-gland-ultrasound-may-lead-to-a-more-accurate-stratification-of-patients-with-the-same-serological-profile-in-sjogrens-syndrome-towards-a-personalized-approach/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/salivary-gland-ultrasound-may-lead-to-a-more-accurate-stratification-of-patients-with-the-same-serological-profile-in-sjogrens-syndrome-towards-a-personalized-approach/