Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) are at increased risk of cardiovascular (CV) disease including heart failure (HF). HF is a heterogeneous condition that is categorized into two main subtypes: HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF). Unlike HFrEF which arises primarily from ischemic myocardial injury, the pathophysiology of HFpEF is less well understood but systemic inflammation is thought to play a role. RA may confer risk of HFrEF via ischemic heart disease and and HFpEF via systemic inflammation, but most prior epidemiologic studies have studied HF in RA as a single entity. Therefore, we sought to investigate the risk of HF and HF subtypes among patients with RA compared to non-RA patients.
Methods: Using an electronic health record (EHR)-based cohort at a large academic U.S. health system, we identified RA patients and non-RA comparators matched by age, sex, and year of entry into the EHR. Index date was defined as the RA diagnosis date (RA cohort) or an encounter date closest to the matched RA patient’s index date (non-RA cohort). The primary outcome was incident HF as ascertained using a previously validated algorithm with a positive predictive value of 90%. HF subtypes were categorized based on EF extracted using natural language processing from clinical notes and cardiology reports closest to the HF incident date (HFpEF, EF ≥ 50%; HFrEF, EF ≤ 40%). Patients with prevalent HF at the index date were excluded. Covariates included age, sex, race, and CV risk factors. Patients were followed from the index date until incident HF, death, last EHR encounter, 20 years of follow up, or end of study (October 26, 2021). We estimated the incidence rate of HF and HF subtypes and used Cox proportional hazards model to estimate the adjusted hazard ratios (HR) for incident HF and HF subtypes.
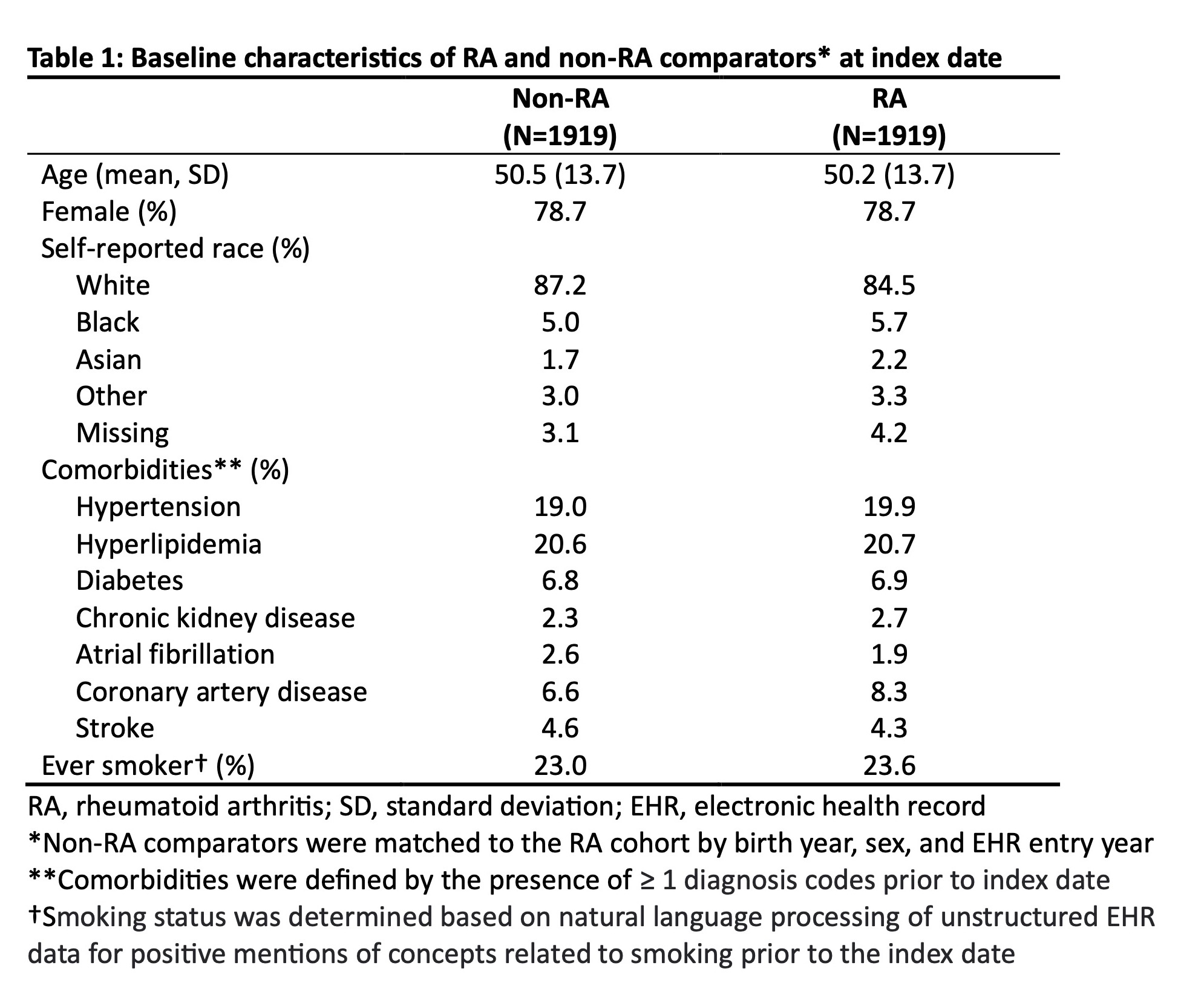
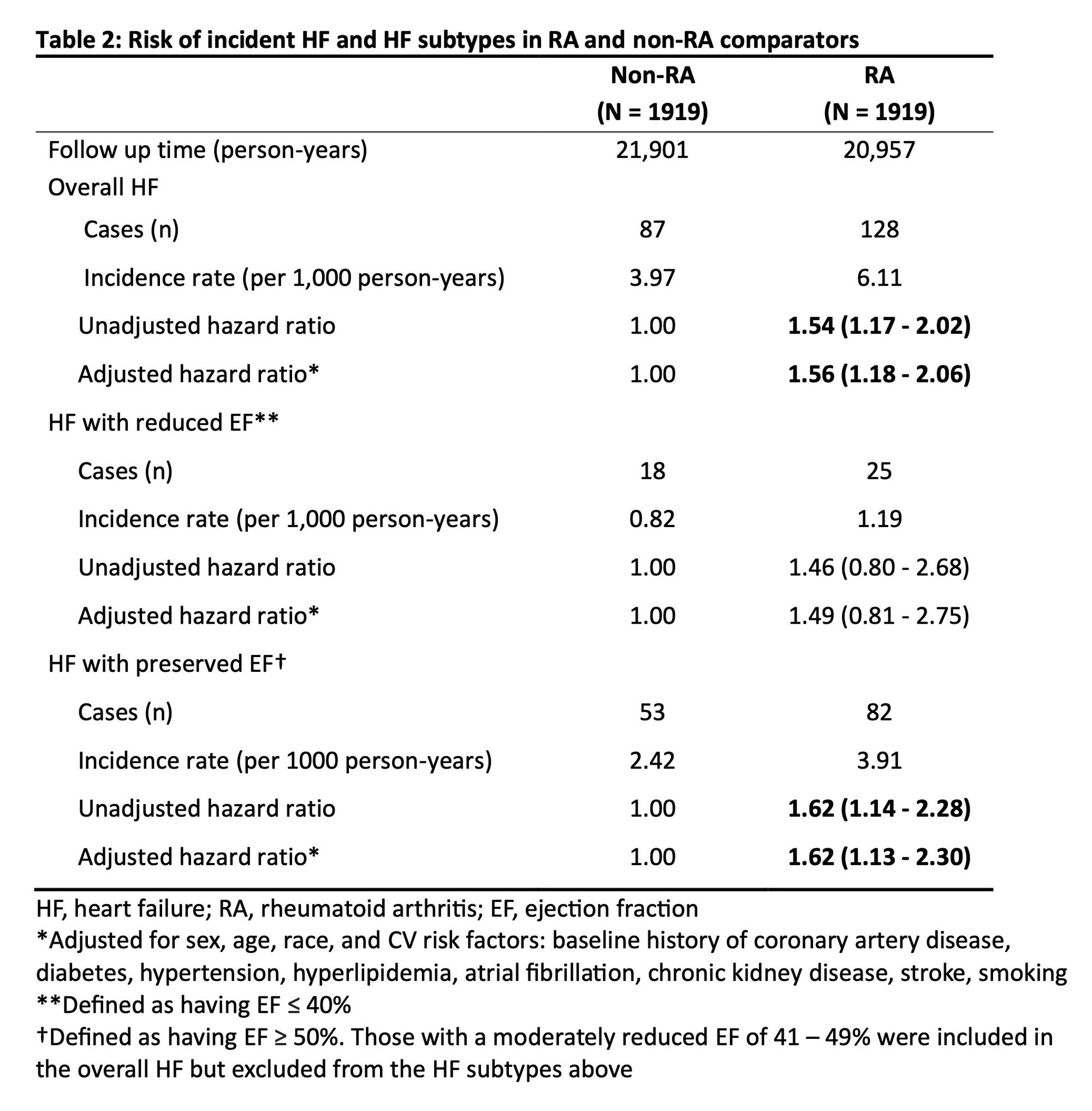
Results: We studied 1919 RA patients and 1919 matched non-RA comparators (mean age 50 years, 78.7% female). Baseline characteristics, including the proportion of patients with CV risk factors, were similar between the two groups (Table 1). Over 42,858 person-years of follow up, we identified 128 incident HF diagnoses (6.7%) in the RA cohort and 87 in the non-RA cohort (4.5%). HFpEF was the most common HF subtype in both cohorts (64.1% in RA, 60.9% in non-RA). The overall incidence rate of HF was higher in the RA cohort than the non-RA cohort (6.11 per 1000 person-years vs. 3.97 per 1000 person-years). Patients with RA had a 56% higher rate of incident HF overall (95% CI: 1.18 – 2.06) compared to those without RA, even after adjusting for established CV risk factors (Table 2). Examining the HF subtypes, we found that RA patients had a 62% higher rate of HFpEF (95% CI: 1.13 – 2.30), but there was no significant difference in HFrEF rate between the RA and non-RA cohorts (95% CI: 0.81 – 2.75).
Conclusion: RA was associated with higher rate of HF overall compared to non-RA comparators, even after adjustment for CV risk factors. The elevated risk was driven by HFpEF, highlighting an opportunity to reduce HF risk in RA by targeting HFpEF. More studies are needed to identify modifiable HFpEF risk factors in RA and methods for earlier detection before clinical HF.
To cite this abstract in AMA style:
Kawano Y, Weisenfeld D, Liu Q, Jeffway M, McDermott G, Dahal K, Stuart J, Joseph J, Cai T, Weber B, Cai T, Liao K. Risk of Incident Heart Failure and Heart Failure Subtypes in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/risk-of-incident-heart-failure-and-heart-failure-subtypes-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-incident-heart-failure-and-heart-failure-subtypes-in-patients-with-rheumatoid-arthritis/