Session Information
Date: Monday, November 8, 2021
Title: Patient Outcomes, Preferences, & Attitudes Poster III: Patient Preferences (1153–1169)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Treatment options for rheumatoid arthritis (RA) have increased dramatically over the past 15 years. The objective of this study was to investigate whether willingness to change treatment and reasons for not changing have shifted by repeating a pivotal study questionnaire 15 years later.1
Methods: Data are from participants with RA enrolled in FORWARD, The National Databank for Rheumatic Diseases, a longitudinal registry of individuals with rheumatic diseases. Patients answered 9 questions on treatment satisfaction and preferences in 2006 (Y06) and/or 2021 (Y21). Questions included an overall assessment of likelihood to change therapy (Q1, “As long as I don’t get worse I wouldn’t want to change my arthritis medications,” rated as true-false) and 8 (Q2-Q9) evaluating reasons for (un)willingness to change (Table 1). Paired McNemar tests were performed in the subset who answered the questionnaire at both Y06 and Y21 to estimate the likelihood of willingness to change therapy at Y21 based on response at Y06. Logistic regression was used to identify predictors at both time points of responses to Q1.
Results: In 2006, 6282 responders had a mean age of 63 years, 17 years RA duration, and exposure to 3 (IQR 2-5) DMARDs. As of April 2021, 1632 responders had a mean age of 66 years, 24 years RA duration, and exposure to 4 (IQR 3-5) DMARDs. Overall for Y06, 64% did not want to change therapy as long as their condition didn’t get worse, compared with 51% from Y21. However, when looking at responses of those who completed both Y06 and Y21 questionnaires (n=442), there were no significant differences in willingness to change therapy. The primary reasons for unwillingness to change therapy over time (Y06 vs Y21) were as follows: satisfaction with medication (53% vs 37%), risk of side effects (72% vs 43%), and doctor recommendation (71% vs 38%) (Table 1). In the paired group, those who provided a reason for not changing in Y21 (eg, side effects) were more likely to have provided the same reason in Y06 (eg, 4.7-fold increase for side effects; Figure 1). Predictors of unwillingness to change therapy in Y06 and Y21 included the following: satisfactory control of RA, risk of side effects, fearing loss of control, doctor thinking current medications were best, and lower levels of pain (Table 2). Predictors related to cost or insurance were associated with unwillingness to change in Y06, but not in Y21.
Conclusion: While the overall proportion of respondents who were unwilling to change therapies was lower in 2021 than in 2006, analysis of those who responded to both questionnaires showed little change. In addition, the major reasons given for not wanting to change therapies did not change from 2006 to 2021, although cost and hassle with insurance companies were no longer significant predictors in 2021. Further data are needed to understand whether the correlation between (un)willingness to change treatments and disease activity and clinical outcomes has evolved over time.
Reference:
1. Wolfe F, Michaud K. Arthritis Rheum 2007;56(7):2135-42.
 Table 1. Treatment predictors and preference for not changing therapy
Table 1. Treatment predictors and preference for not changing therapy
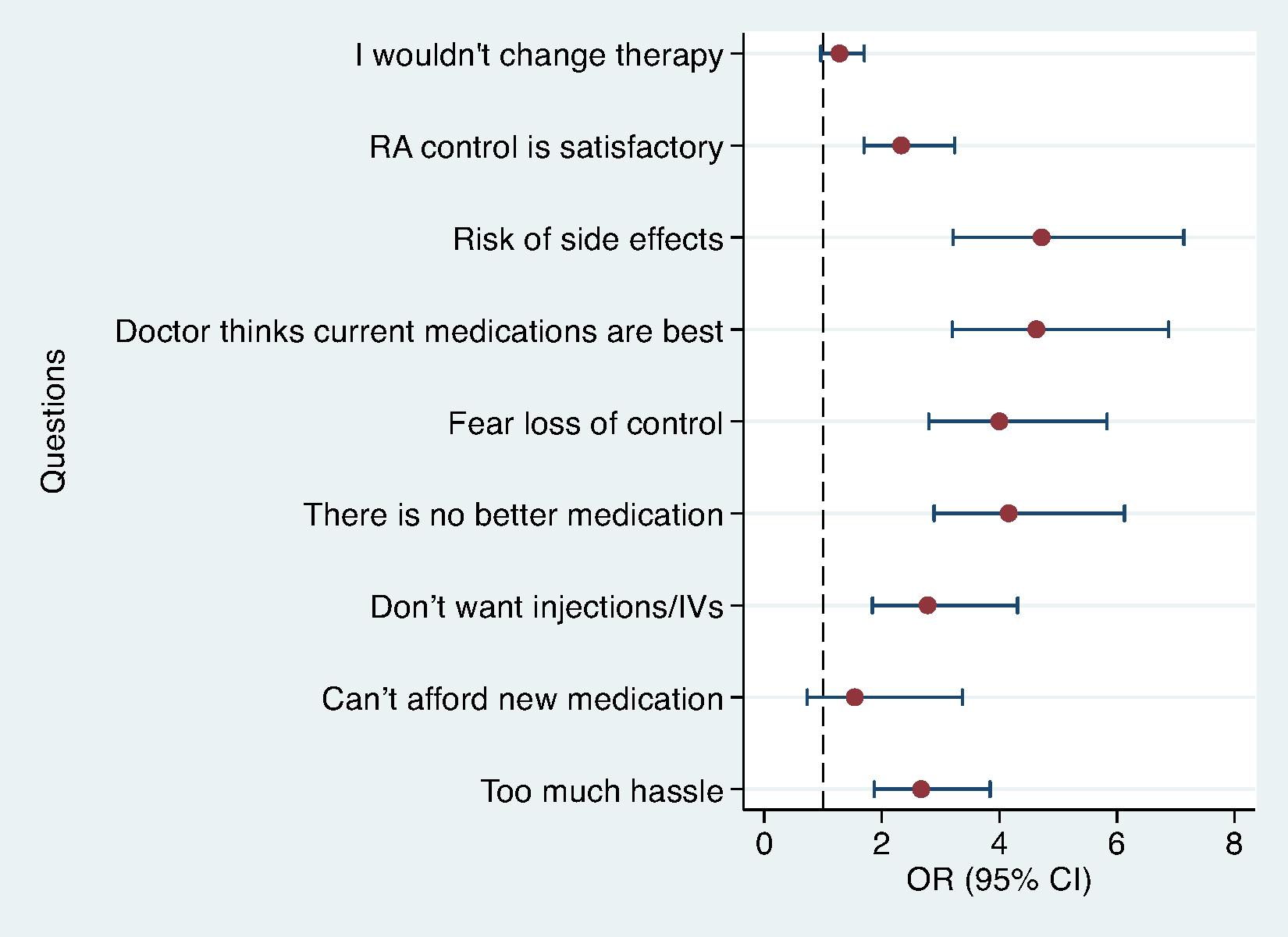 Figure 1. Odds (95% CI) of being unwilling to change medications at Y21 if unwilling to change at Y06.
Figure 1. Odds (95% CI) of being unwilling to change medications at Y21 if unwilling to change at Y06.
 Table 2. Multivariable predictors of unwillingness to change therapy outcome in overall and paired samples.
Table 2. Multivariable predictors of unwillingness to change therapy outcome in overall and paired samples.
To cite this abstract in AMA style:
Michaud K, Pedro S, Jasion V, Budlong H, Suboticki J, Wolfe F, Katz P. Resistance of Patients with Rheumatoid Arthritis to Changing Therapy: A 15-year Follow-up [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/resistance-of-patients-with-rheumatoid-arthritis-to-changing-therapy-a-15-year-follow-up/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/resistance-of-patients-with-rheumatoid-arthritis-to-changing-therapy-a-15-year-follow-up/
