Session Information
Date: Sunday, November 8, 2020
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: African Americans [AA] and minorities in the lower socioeconomic strata of Chicago are disproportionately affected by pulmonary sarcoidosis, and regularly exposed to poorer air quality than Caucasians [C]. Histopathologically, sarcoidosis is characterized by granulomatous inflammation, and elevated serum angiotensin converting enzyme (sACE) are observed in about 75% of untreated patients with sarcoidosis, in part due to macrophage activation. Though the etiology remains unknown, exposure via antigen inhalation has been posited to evoke this inflammatory immune response. In this study, we examine the relationship between particulate matter air pollution and sarcoidosis inflammation and hypothesize that poor air quality indices are associated with sACE.
Methods: A cohort of female patients from the University of Illinois at Chicago lung disease registry residing in the Chicago area with sarcoidosis and documented sACE levels (2010-2015) was evaluated retrospectively. Demographic and clinical variables were abstracted from the medical record. ACE levels ≥ 50 U/L were considered elevated and inflammatory. Daily AQI measurements were obtained from the USA EPA database during a 6-month interval prior to ACE level measurement. Residential AQI levels were interpolated from the 5 nearest pollution monitors to a patient’s residence by inverse distance weighting with a power of 2 (R-package “phylin”) and maximum average AQI levels at 10-day intervals were calculated. Demographic/clinical parameters were compared among AA and C groups and the risk of elevated sACE at the end of the 6-month interval was estimated by Cox proportional hazard ratio models (R-package “survival”).
Results: We identified 32 female patients (AA=21, C =11) in the study period. sACE levels between AA and C and baseline demographics were similar at the time of sACE measurement (MWU-test p-val >0.05). Evaluation of environmental factors, AQI and smoking history on ACE level, adjusted for time from sarcoidosis diagnosis, revealed a significant hazard reduction of elevated sACE levels by 2% for every unit increase in AQI in AA (Figure 1A, Log-Rank p-val=0.002). Contrastingly, in C, current or former smoking history, not AQI, was associated with reduced risk of elevated ACE levels (Figure 1B, Log-Rank p-val=0.005). At time of ACE level measurements, a trend of increased utilization of systemic immunosuppressive therapy was observed in AA (χ2 p-val=0.053, odds ratio=5).
Conclusion: A paradoxical association between inflammatory activity in sarcoidosis and environmental factors that may increase antigenic exposure was identified. It is possible that AA and C females show different phenotypes of sarcoidosis and respond distinctly to inhaled antigens. In AA females, a higher AQI was linked to lower ACE levels while in C, current or former smoking status was linked with lower ACE levels. Further studies are needed to expound underlying mechanisms of these associations; however, our data supports the idea that inhaled antigenic stimuli are directly related with sarcoidosis inflammatory activity and suggest that some antigens may downregulate granulomatous inflammation.
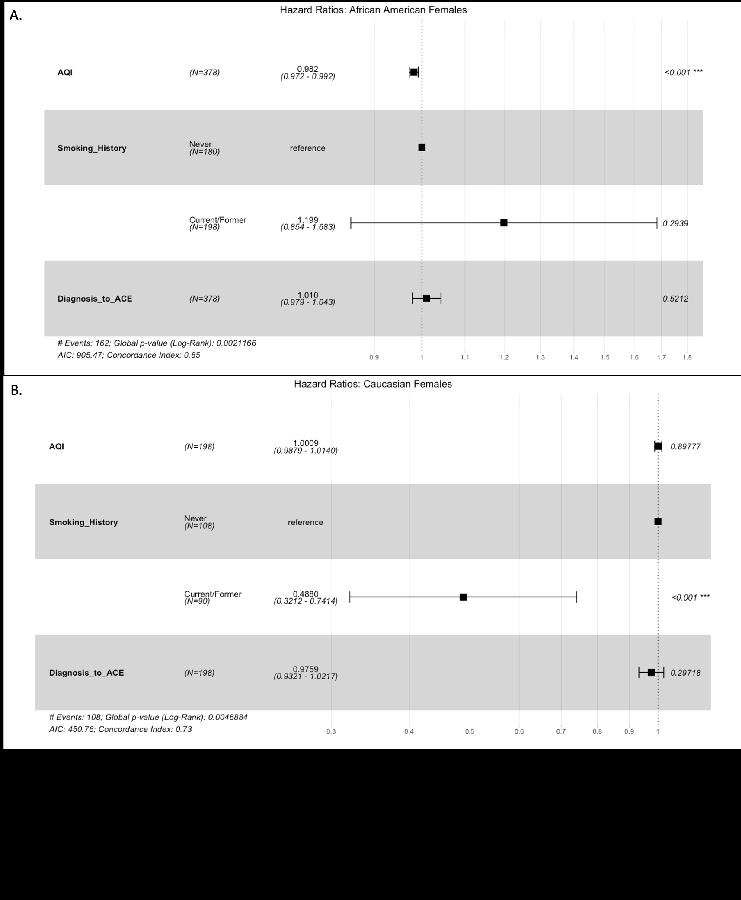 Figure 1. Forest plot demonstrating the Cox proportional hazard ratio and 95% confidence intervals associated with risk of angiotensin converting enzyme (ACE) levels over 50 U/L in (A) African American and (B) Caucasian females. In African American females, unit increments in air quality index (AQI) are associated with a 2% hazard reduction of elevated ACE levels at 6 months. In African Americans, smoking history and time from diagnosis of sarcoidosis (in years) to ACE level are not associated with increased ACE levels. Contrastingly, in Caucasian females, current or former smoking history is associated with a hazard reduction of 51% of elevated ACE levels. In Caucasians, AQI and time from years from diagnosis of sarcoidosis to ACE are not associated with ACE levels.
Figure 1. Forest plot demonstrating the Cox proportional hazard ratio and 95% confidence intervals associated with risk of angiotensin converting enzyme (ACE) levels over 50 U/L in (A) African American and (B) Caucasian females. In African American females, unit increments in air quality index (AQI) are associated with a 2% hazard reduction of elevated ACE levels at 6 months. In African Americans, smoking history and time from diagnosis of sarcoidosis (in years) to ACE level are not associated with increased ACE levels. Contrastingly, in Caucasian females, current or former smoking history is associated with a hazard reduction of 51% of elevated ACE levels. In Caucasians, AQI and time from years from diagnosis of sarcoidosis to ACE are not associated with ACE levels.
To cite this abstract in AMA style:
Case A, Fraidenburg D, Rubinstein I, Ascoli C. Relationship Between Air Quality and Sarcoidosis Inflammatory Activity [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/relationship-between-air-quality-and-sarcoidosis-inflammatory-activity/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-air-quality-and-sarcoidosis-inflammatory-activity/
