Session Information
Date: Monday, November 8, 2021
Title: Plenary III (1424–1429)
Session Type: Plenary Session
Session Time: 11:15AM-11:30AM
Background/Purpose: The risks of death and of type 2 diabetes mellitus (T2DM) are increased in RA mainly due to inflammation mediated accelerated cardiovascular disease (CVD) and insulin resistance. In the general population, statins reduce CVD and mortality with a slight increase in T2DM risk. We aimed to assess CVD and mortality benefits and T2DM risk with statins in RA patients.
Methods: We conducted a prevalent new-user cohort study within the UK Clinical Practice Research Datalink, the Hospital Episode Statistics [HES] and Office of National Statistics [ONS] databases. The cohort included individuals ≥18 years old who had a 1st diagnosis of RA and ≥1 DMARD use with no alternative diagnoses and ≥1 year baseline data between 1989 and 2018. Patients with prior DM and no HES/ONS linkage were excluded for T2DM and CVD/mortality cohorts, respectively. Statin initiators were matched with non-users (1:2) on the time-conditional propensity score (TCPS) that included age, sex, BMI, smoking, alcohol, joint surgeries, prior CVD, hypertension, rheumatic diseases comorbidity index, osteoporosis/fractures, cancer, thyroid, chronic liver, kidney, lung and other heart diseases, healthcare utilization, DMARDs, glucocorticoids, NSAIDs, and CVD medications (DM and ethnicity for CVD/mortality). The subjects were followed up for the outcomes of CVD (myocardial infarction, stroke, hospitalized heart failure, CVD death), all-cause mortality and T2DM (diagnostic codes or prescription of antidiabetics). The risk of outcomes was estimated using Cox proportional hazards with adjustment for deciles of TCPS and imbalanced patient characteristics after matching.
Results: The study included 1768 statin initiators and 3528 non-users for CVD/mortality; 3608 statin initiators and 7208 non-users for T2DM (Figure). Baseline characteristics of the statin initiators and non-users in the matched cohort were balanced except for DM, some medications and prior cerebrovascular disease (Table 1). Among 1768 statin initiators and 3528 non-users, 63 vs. 340 CVD (3.0/100 person-years [PY] vs. 2.7/100 PY) and 62 vs. 525 deaths (2.7/100 PY vs. 4.1/100 PY) occurred, respectively (Table 2). Incident T2DM was noted in 128 of 3608 statin initiators (3.0/100 PY) and 518 of 7208 non-users (2.0/100 PY). Statin initiation was associated with 32% (HR=0.68, 95% CI 0.51-0.90) reduction in CVD, 54% (HR=0.46, 95% CI 0.35-0.60) reduction in all-cause mortality, and 33% increase in T2DM (HR= 1.33, 95% CI 1.09-1.63) risks. Number needed to treat (NNT) to prevent a CVD and mortality in 1-year was 102 and 42, respectively. Number needed to harm (NNH) for a new T2DM was 127. Patients with and without prior CVD had similar CVD (36% vs. 34%) and mortality (62% vs. 54%) reduction with statins (Table 2).
Conclusion: Statins are associated with important reductions in CVD and mortality in both primary and secondary CVD prevention, with a modest increase in T2DM risk in RA patients. The resulting NNT/NNH suggest that CVD/mortality benefits of statins outweigh T2DM risk.
 Figure. Overview of the study design and cohort creation for outcomes of cardiovascular disease (CVD), all-cause mortality and type 2 diabetes mellitus (T2DM)
Figure. Overview of the study design and cohort creation for outcomes of cardiovascular disease (CVD), all-cause mortality and type 2 diabetes mellitus (T2DM)
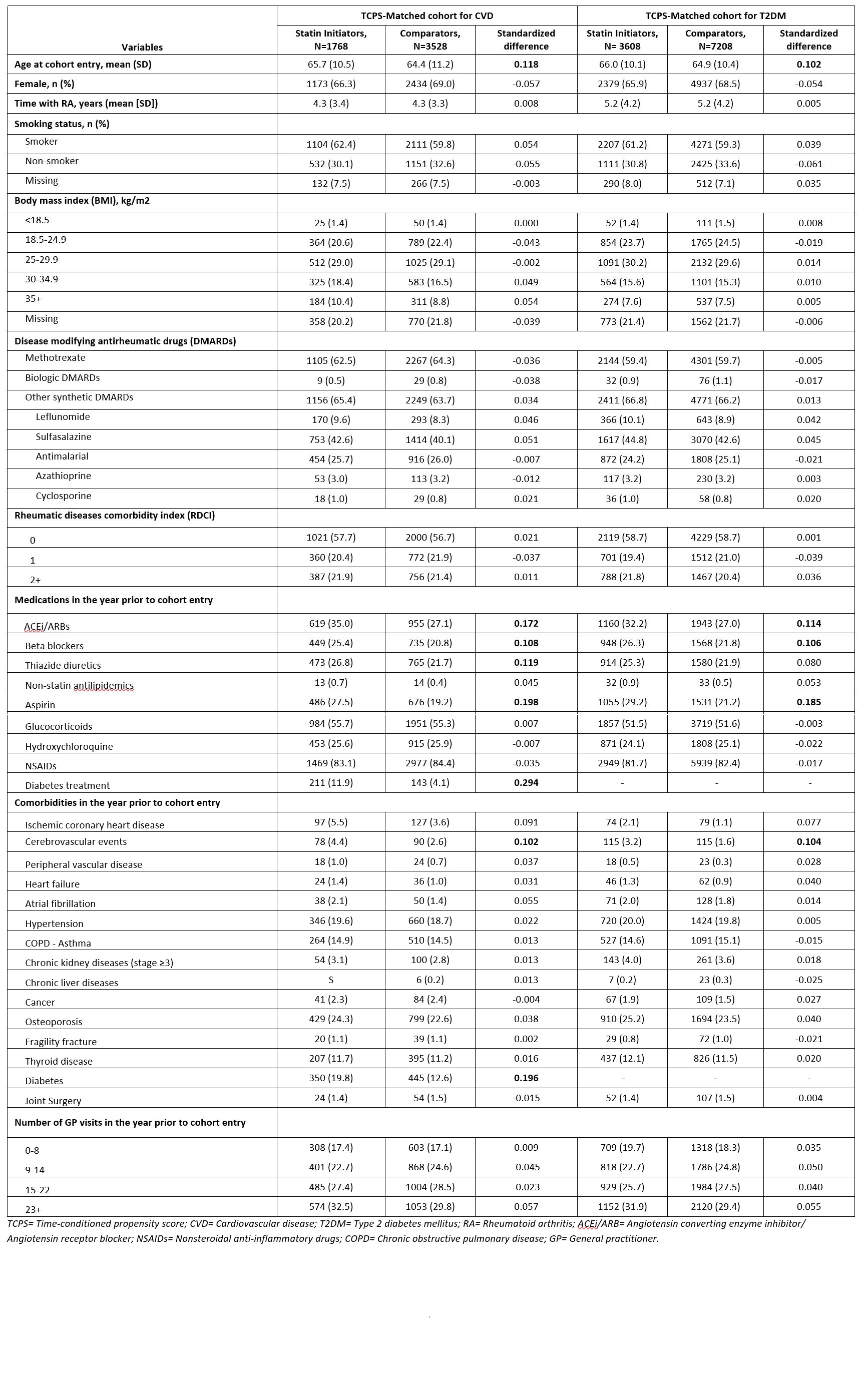 Table 1. Baseline characteristics of propensity score matched cohorts
Table 1. Baseline characteristics of propensity score matched cohorts
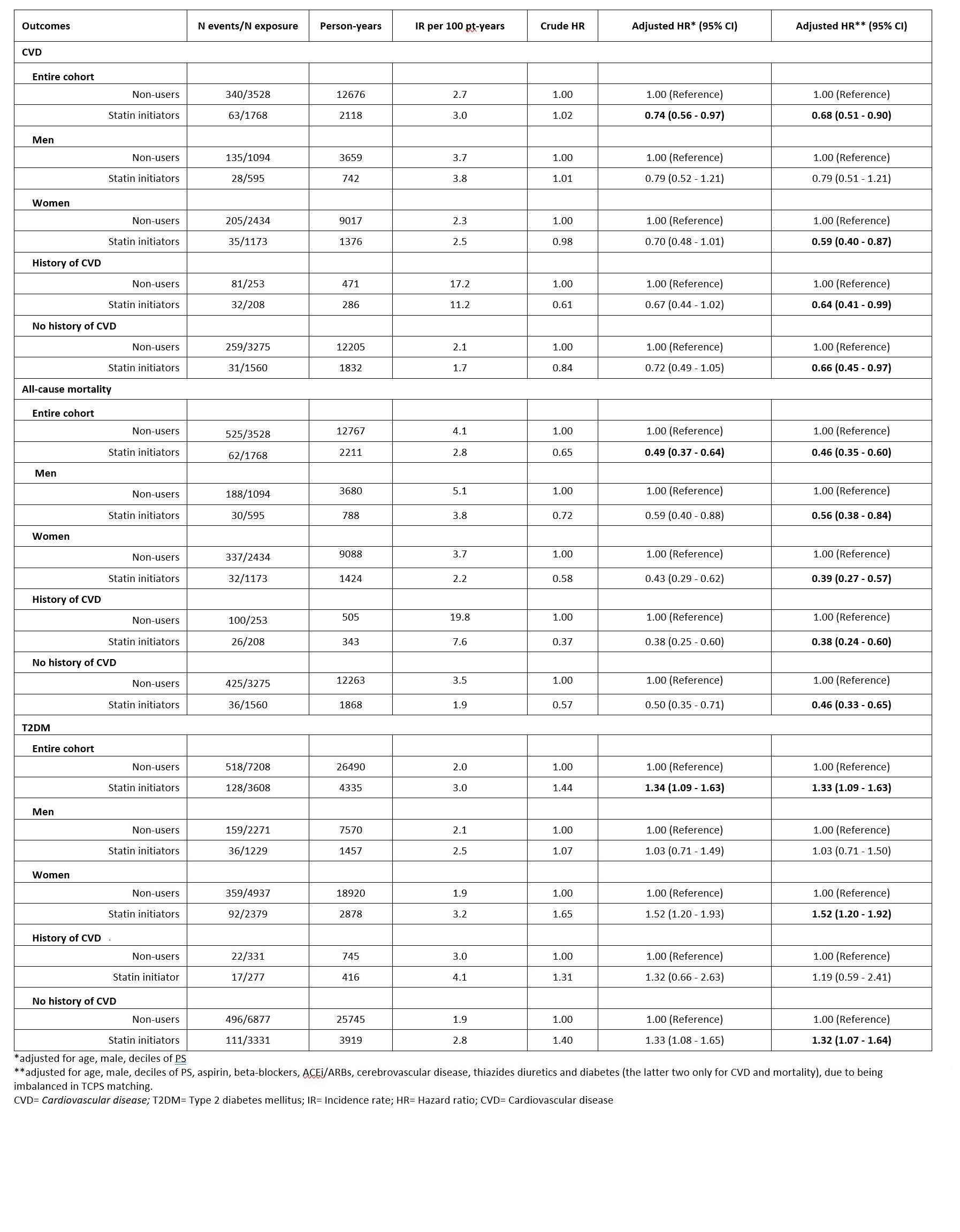 Table 2. Association between statin initiation and CVD, all-cause mortality and T2DM
Table 2. Association between statin initiation and CVD, all-cause mortality and T2DM
To cite this abstract in AMA style:
Ozen G, Dell’Aniello S, Pedro S, Michaud K, Suissa S. Reduction of Cardiovascular Disease and Mortality versus Risk of New Onset Diabetes with Statin Use in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/reduction-of-cardiovascular-disease-and-mortality-versus-risk-of-new-onset-diabetes-with-statin-use-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/reduction-of-cardiovascular-disease-and-mortality-versus-risk-of-new-onset-diabetes-with-statin-use-in-patients-with-rheumatoid-arthritis/
