Session Information
Date: Sunday, November 13, 2022
Title: Systemic Sclerosis and Related Disorders – Clinical Poster II
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Digital ischemic complications (DICs, including digital ulcers, digital pitting/scars, gangrene and/or amputation) can significantly impact hand function, disability and overall prognosis in SSc. We aimed to study the prevalence and risk factors for DICs in SSc and compared treatment patterns among patients with and without DICs.
Methods: A cohort of SSc patients meeting ACR/EULAR 2013 criteria evaluated at our institution between Jan 2001-Dec 2018 was assembled. Demographics, clinical characteristics, laboratory tests, treatment for Raynaud’s, use of antiplatelet (aspirin 81 mg), statin therapy and occurrence of DICs were abstracted. DOAD on Laser doppler flowmetry (LDF) was present if pre- and post-warming skin blood flow was ≤206 arbitrary units. Severity of DOAD was assessed based on number of digits involved. Macrovascular disease was defined as stenosis/occlusion involving palmar arch, ulnar, radial, brachial, axillary and/or subclavian arteries on duplex US. Risk factors associated with DICs in SSc and their associations with vasodilator, antiplatelet and statin therapy were evaluated.
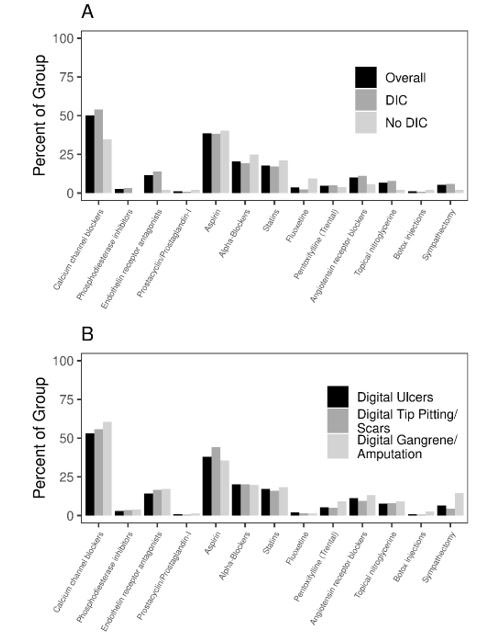
Results: We identified 273 SSc patients (mean age 57.5 ± 13.3 y, 81% female, 93% Caucasian). Mean disease duration was 4.8±7.1 y. The majority had limited cutaneous SSc (lcSSc) (78%) and 67% had a positive SSc specific antibody. Cohort characteristics are described in Table 1. 217/273 (79%) patients experienced 1 or more DICs (digital ulcers in 203, digital pitting/scar in 138, digital gangrene in 76). Patients with DICs had a significantly higher prevalence of DOAD (89% vs 54%, p< 0.001), macrovascular disease (32% vs 9%, p< 0.001), ILD (41% vs. 27%, p=0.04), calcinosis (95/192 (49%) vs. 7/44 (16%), p< 0.001), and pericardial effusion (25% vs. 12%, p=0.047), than those without DICs. No difference was noted in regard to skin severity, smoking, BMI, hypertension, hyperlipidemia, diabetes, coronary artery disease, telangiectasias, pulmonary hypertension, renal crisis, GI dysmotility or myositis. Treatment patterns among patients with and without DICs are described in Figure 1. Calcium channel blocker (CCB) and phosphodiesterase 5 inhibitor (PDE5I) use was significantly higher among SSc patients with DICs than those without DICs (CCBs: 53% vs. 34%, p=0.01; PDE5: 29% vs. 2%, p=0.01) likely due to confounding by indication. The use of antiplatelet therapy or statins was not associated with DICs, even after adjusting for cardiovascular risk factors (ASA: OR 0.83, 95% CI 0.45-1.54; statin OR 0.67, 95% CI 0.28-1.62).
Conclusion: Our study confirms a high prevalence of DICs in SSc, with digital ulcers occurring in nearly 75% patients. A higher risk of DICs is associated with DOAD on LDF, macrovascular disease on duplex ultrasonography, ILD, calcinosis and pericardial effusion. While there is a significantly higher utilization of vasodilators among patients with DICs given their known efficacy, the utilization of antiplatelet therapy and statins was not different among these groups. Whether this suggests a lack of evidence supporting their use in clinical practice, or inefficacy in preventing DICs remains unclear and warrants further study.
To cite this abstract in AMA style:
Makol A, Hinze A, Giblon R, Radwan Y, Gunderson T, Liedl D, Warrington K, Crowson C, Wennberg P. Prevalence, Risk Factors and Treatment Patterns of Digital Ischemic Complications in Systemic Sclerosis: A Single Center Cross-Sectional Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/prevalence-risk-factors-and-treatment-patterns-of-digital-ischemic-complications-in-systemic-sclerosis-a-single-center-cross-sectional-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-risk-factors-and-treatment-patterns-of-digital-ischemic-complications-in-systemic-sclerosis-a-single-center-cross-sectional-study/