Session Information
Date: Tuesday, November 14, 2023
Title: (1913–1944) Miscellaneous Rheumatic & Inflammatory Diseases Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: The prevalence of comorbidities in rheumatic diseases may vary by disease and geographic region. This study aimed to investigate the comorbidities associated with rheumatoid arthritis (RA), ankylosing spondylitis (AS), primary Sjögren’s syndrome (PSS) and systemic lupus erythematosus (SLE).
Methods: Data from consecutive patients attending a tertiary care facility between 2020 and 2021 were analyzed. Patients diagnosed with RA, AS, PSS and SLE based on established criteria were included in the study
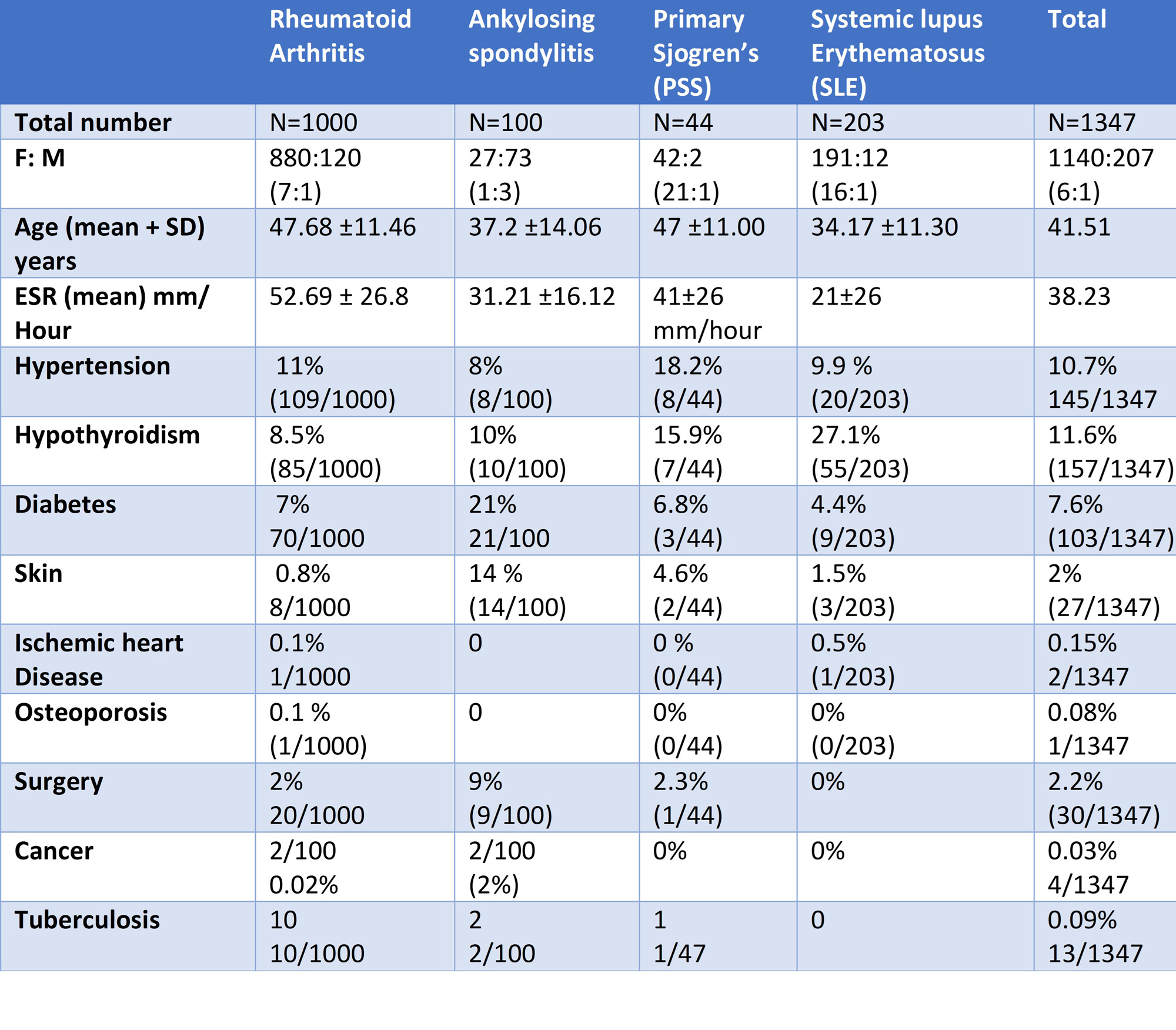
Results: A total of 1347 patients (Table 1) were analyzed in this study. In patients with inflammatory rheumatic diseases (N=1347), hypertension (10.7%) and hypothyroidism (11.6%) were the most common comorbidities. When individually assessed for specific diseases, patients with rheumatoid arthritis (RA) (N=1000) had hypertension as the most common comorbidity (11%), followed by hypothyroidism (8.5%). Likewise, patients with ankylosing spondylitis (AS) (N=100) showed a similar pattern, with hypertension and hypothyroidism being the most common comorbidities. Patients with Sjögren’s syndrome (N=44) showed a higher prevalence of hypertension (18.2%) and hypothyroidism (15.9%). In patients with systemic lupus erythematosus (SLE) (N=203), the prevalence of hypothyroidism (27.1%) and hypertension (9.9%) was higher, while diabetes was less common The overall prevalence of hypertension ranged from 8 to 12%, with the highest prevalence being found in primary Sjögren’s syndrome (18.2%). SLE had the highest prevalence of hypothyroidism (27.1%), which was two to three times higher compared to other rheumatic diseases, likely reflecting the increased incidence of autoimmune thyroiditis in this population. In contrast, the prevalence of diabetes was lower in SLE, possibly reflecting the younger age of the patients. The relatively younger age group may also explain the lower prevalence of comorbidities such as cancer, osteoporosis, and ischemic heart disease in the study population Overall, the prevalence and pattern of comorbidities in this study were relatively lower compared to internationally published studies that included populations from different ethnic backgrounds. These findings underscore the distinct patterns of comorbidities among various rheumatic diseases, likely influenced by underlying disease characteristics. Additionally, the younger age group in the study population with fewer comorbidities emphasizes the importance of early diagnosis and optimal management of rheumatic diseases to prevent the development of comorbidities.
Conclusion: Prevalence and pattern of comorbidities in rheumatic diseases vary between different diseases and populations. Understanding these differences is crucial for tailoring treatment strategies and improving patient outcomes.
To cite this abstract in AMA style:
Ramteke S, Ramteke s, Yadav S. Prevalence and Patterns of Comorbidities in Different Rheumatic Diseases: A Study from Tertiary Healthcare Centre [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-patterns-of-comorbidities-in-different-rheumatic-diseases-a-study-from-tertiary-healthcare-centre/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-patterns-of-comorbidities-in-different-rheumatic-diseases-a-study-from-tertiary-healthcare-centre/