Session Information
Date: Sunday, November 7, 2021
Title: Epidemiology & Public Health Poster II: Inflammatory Arthritis – RA, SpA, & Gout (0560–0593)
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Several types of lung diseases complicate the rheumatoid arthritis (RA) disease course such as interstitial lung disease (ILD) and obstructive lung diseases. The prevalence of lung diseases varies substantially across studies, and there remains a poor understanding of the progression of lung diseases early in the RA disease course. We aimed to identify the prevalence and early progression of lung diseases in patients with recently diagnosed RA.
Methods: We performed a prospective cohort study of lung diseases in recently-diagnosed RA patients at an academic center from 2017-2021. Patients fulfilled the 2010 ACR criteria for RA and were diagnosed within the prior two years. At baseline and 1-year follow-up visits, patient-reported outcomes measures (e.g. Modified Research Council [MRC] dyspnea scale and Health Assessment Questionnaire), clinical assessments (e.g. DAS28-ESR), and complete pulmonary function tests (PFTs) were collected. At the initial visit, a high-resolution computed tomography (HRCT) scan of the lungs was completed with thin (1.25 mm) slices with prone and supine imaging. HRCTs were scored semi-quantitatively in 6 lung regions by an expert chest radiologist blinded to clinical data.
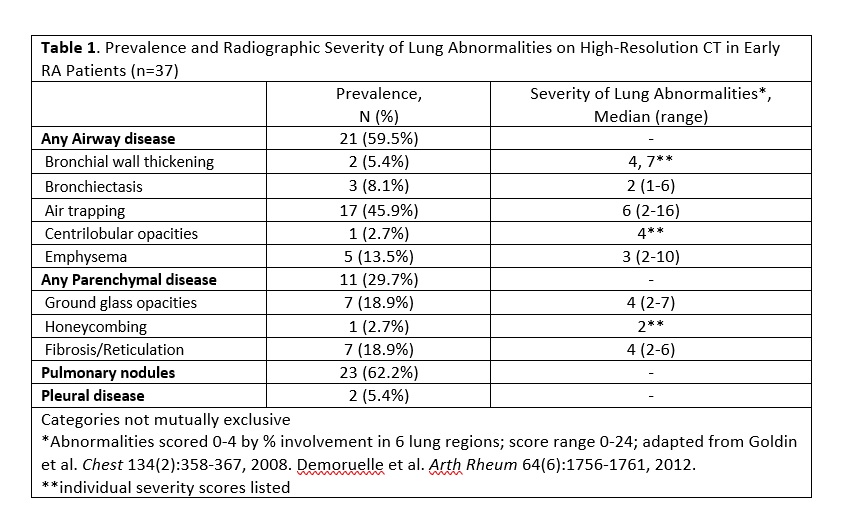
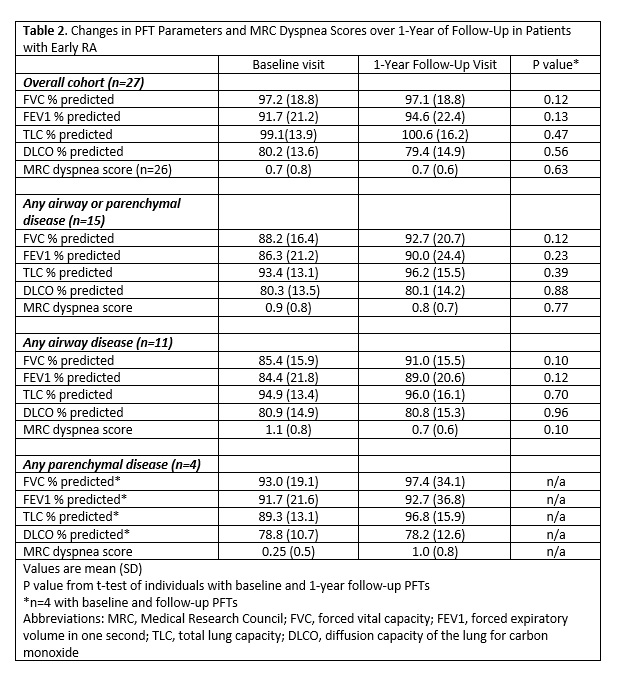
Results: Among 37 recently-diagnosed RA patients, mean age was 57.2 (SD 11.9) years, and the majority were female (81.1%), white (81.1%), seropositive (83.8% RF, 86.5% anti-CCP), and MTX treated (81.1%). Cigarette smoking history was present in 59.5%, but a minority of patients had clinically-diagnosed lung disease (5.4% COPD, 10.8% asthma, 2.7% ILD). Despite 86.5% of subjects reporting no or only slight dyspnea (MRC grade 0 or 1), 29.7% had evidence of parenchymal disease, 59.5% had evidence of airway disease, and 62.2% had pulmonary nodules on HRCT (Table 1). Semiquantitative HRCT scoring revealed most airway and parenchymal abnormalities to be mild in severity. Similarly, physiologic impairment on PFTs was infrequent with 16.2% demonstrating restrictive and 18.9% obstructive spirometry. Among patients who have completed 1-year of follow-up (n=27), there was no significant change in PFT parameters (FEV1, FVC, TLC, DLCO) or MRC score (Table 2). Stability in PFTs was present even among RA patients with detectable lung disease on HRCT. Baseline DAS28-ESR was negatively correlated with FVC (r = -0.42, p = 0.01) and positively correlated with MRC scores (r=0.57, p< 0.001), but not with other PFT parameters or with HRCT findings. Seropositivity for RF or anti-CCP antibody was not associated with an increase in airway or parenchymal abnormalities.
Conclusion: In this prospective cohort of patients with recently-diagnosed RA who underwent systematic evaluation for lung disease, airway and parenchymal abnormalities were commonly detected on HRCT but mild in severity. Pulmonary nodules were the most detected HRCT finding. Physiologic impairment was infrequent, and the stability of PFTs and dyspnea symptoms early after RA diagnosis is reassuring and may suggest that patients with asymptomatic imaging findings do not require treatment modifications, though longer follow-up periods are needed.
To cite this abstract in AMA style:
Mahajan T, Hershberger D, Devries M, Roul P, Yang Y, Edwards S, Thiele G, Mikuls T, O'Dell J, England B. Prevalence and Early Progression of Lung Diseases in Patients with Recently-Diagnosed Rheumatoid Arthritis: A Prospective Cohort Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/prevalence-and-early-progression-of-lung-diseases-in-patients-with-recently-diagnosed-rheumatoid-arthritis-a-prospective-cohort-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prevalence-and-early-progression-of-lung-diseases-in-patients-with-recently-diagnosed-rheumatoid-arthritis-a-prospective-cohort-study/