Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Children with oligoarticular JIA are at increased risk of developing uveitis. JIA category, ANA positivity, ≤4 years JIA duration, and < 6 years old at diagnosis are known risk factors. Regular ophthalmic examination is important for screening since uveitis is asymptomatic. Tear fluid is easily obtained and has been used for biomarker studies. This pilot study aims to identify potential tear-based inflammatory markers that can differentiate children with JIA who develop uveitis.
Methods: This prospective cohort study at Cincinnati Children’s compared children with JIA-associated uveitis (JIA-U) and JIA without uveitis (JIA-no-U) with oligoarticular subtype. Medical charts were reviewed for demographics, uveitis characteristics, ophthalmic examination, and current treatment. Tear fluid was collected by Schirmer strips. We used advanced proteomic strategies (isobaric tag for relative quantitation [iTRAQ] labeling and nanoLC-MS/MS) to quantify proteins in the left eye of patients with JIA-U and JIA-no-U in duplicate. In those with unilateral JIA-U, the affected eye was used. We reported the log of the mean of the ratios derived from two abundance readings per protein for each subject. Based on a Wilcoxon rank sum exact test we considered a P-value < 0.1 to be significant.
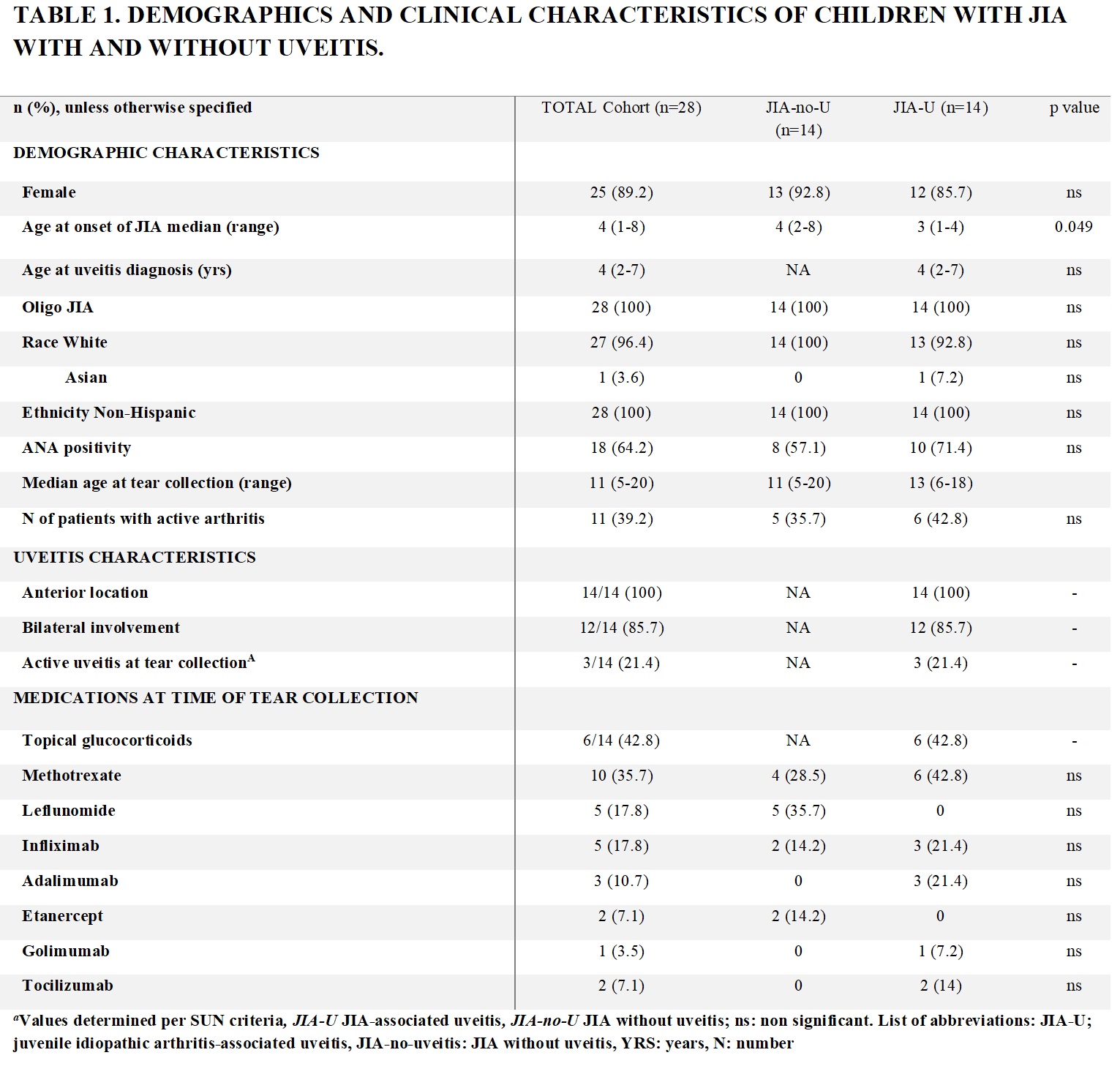
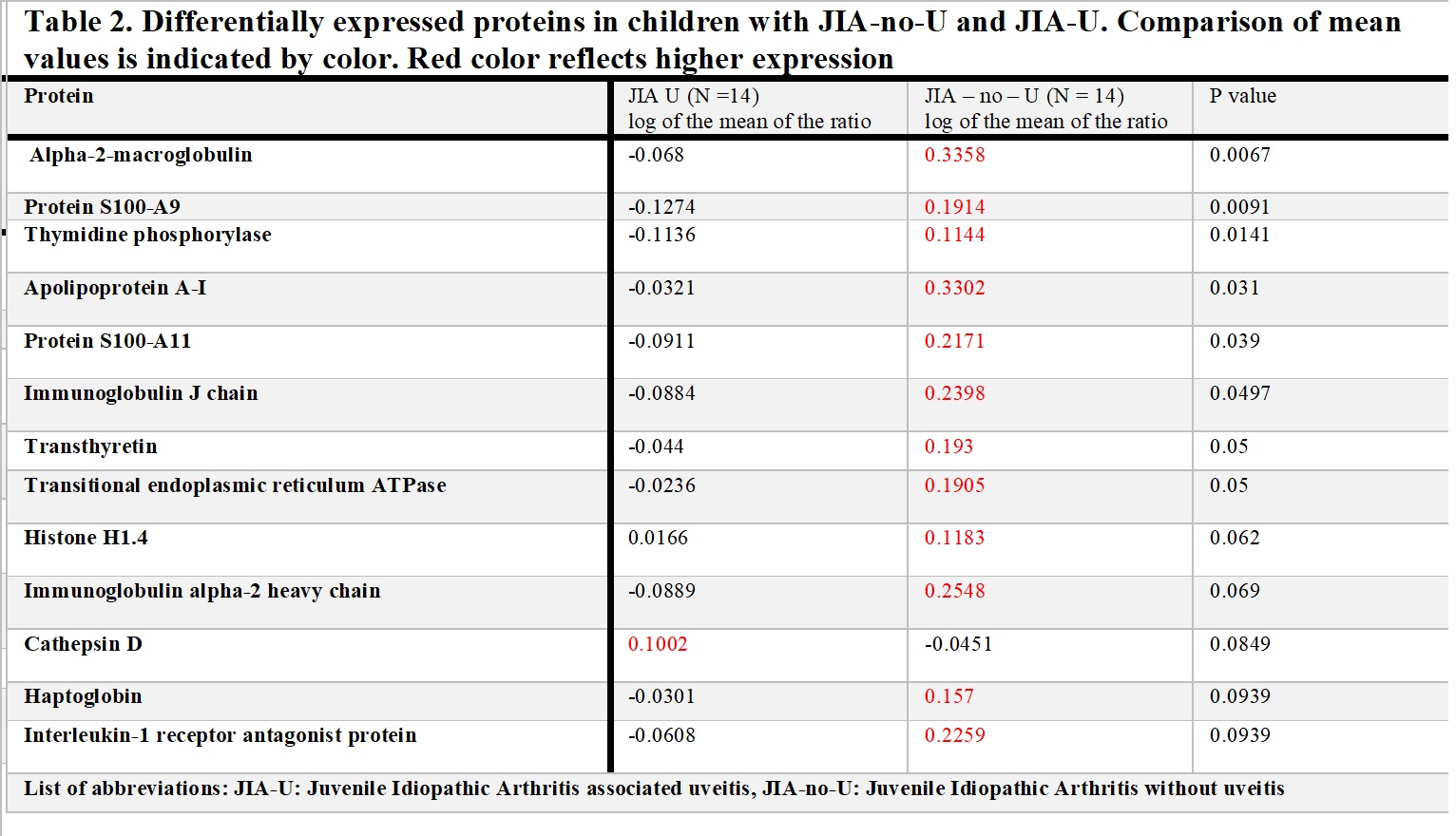
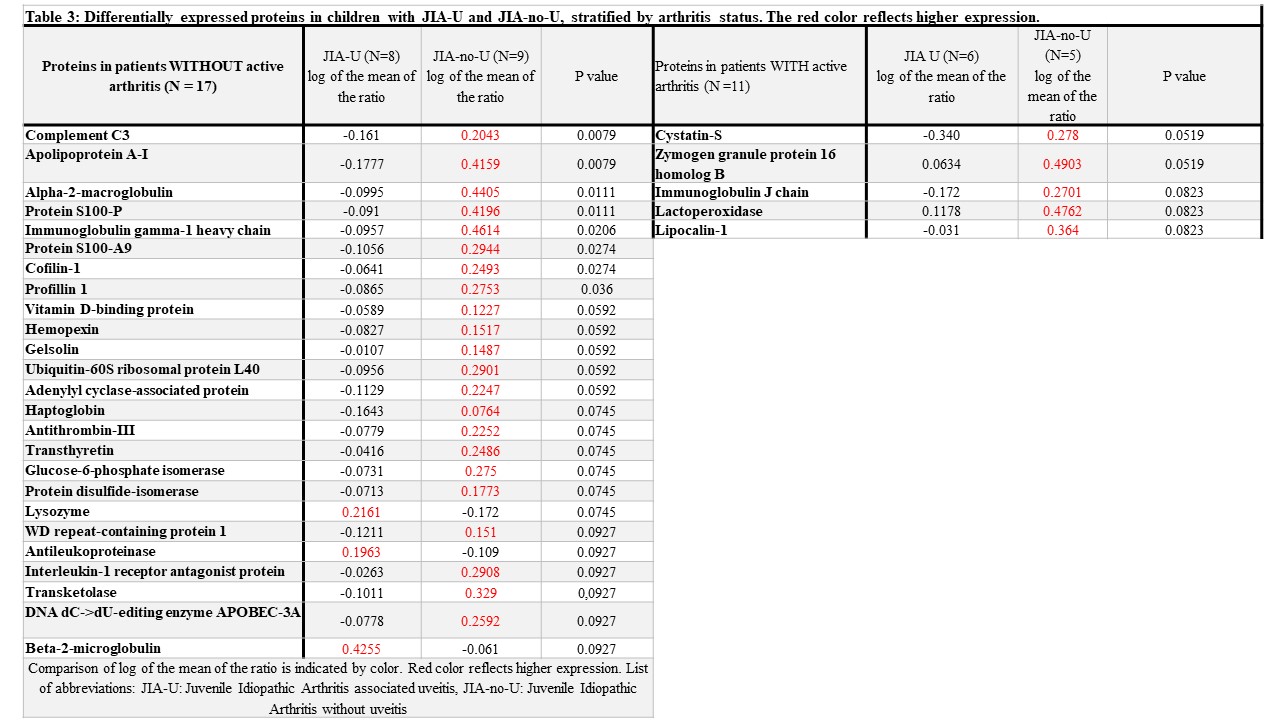
Results: Tear samples of 28 JIA patients were collected (14 JIA-U and 14 JIA-no-U). Demographic and clinical characteristics are summarized (Table 1). Thirteen proteins exhibited differences in tears of 14 children with JIA-U and 14 with JIA-no-U (Table 2). Of these, 8 showed a difference at p≤0.05. All the proteins were higher in the group of JIA-no-U except for cathepsin D. Cathepsin D and Transitional endoplasmic reticulum ATPase have been associated with the retinal pigment epithelium (RPE) and maintaining the blood-retinal barrier (BRB). As 39% of patients had active arthritis at the time of tear collection, we stratified the analysis by arthritis activity as joint inflammation could affect the presence and level of inflammatory mediators (Table 3). A larger number of proteins differentiated patients with JIA-U and JIA-no-U p who had inactive arthritis (Table 3). Specifically, complement 3, apolipoprotein, S100 proteins, transthyretin, and beta-2 microglobulin have been associated with uveitis.
Conclusion: Uveitis is a vision-threatening disease that warrants exploration of techniques for early detection and treatment. The eye is an immune-privileged organ immunologically shielded by the RPE as part of the BRB. We hypothesize that the immune response proteins identified within the tears of JIA-U patients are by-products of inflammation-induced RPE and BRB breakdown, promoting the inflammatory cascade. Tears of children with JIA-U and JIA-no-U display differential expression of proteins, but it seems to be influenced by arthritis activity. Further study in larger cohorts is needed to verify these results.
To cite this abstract in AMA style:
Maccora I, Altaye M, Nguyen T, Greis K, Haffey W, Hennard T, Sproles A, Thornton S, Miraldi Utz V, Angeles-Han S. Potential Tear-Based Uveitis Biomarkers in Children with JIA: A Pilot Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/potential-tear-based-uveitis-biomarkers-in-children-with-jia-a-pilot-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/potential-tear-based-uveitis-biomarkers-in-children-with-jia-a-pilot-study/