Session Information
Date: Monday, November 9, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster III: Bench to Bedside
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Platelet-bound complement activation products (PC4d), defined as PC4d20 net mean fluorescent intensity [MFI], or a thrombotic risk score that includes PC4d, C3 and anti-phosphatidylserine/prothrombin antibodies (anti-PS/PT IgG) (1) correlate with venous thromboses in SLE. The current study was initiated to further evaluate the association between PC4d and arterial and venous thrombotic events.
Methods: Using a cross-sectional design, we examined the association of PC4d, measured by flow cytometry, with thrombosis. PC4d was dichotomized and we evaluated the ability of different cutoff values, ranging from 5 to 20 net MFI, to discriminate for the history of vascular events. The thrombotic risk was calculated as previously described (1).
Results: 150 SLE patients (40 ±13 years old, 91% female, 33% Hispanic, 26% African American) were included; 38% had antiphospholipid antibodies (aPL). Thirty-one vascular events (18 venous, 13 arterial) occurred within five years of study enrollment. Arterial and venous events, as compared to no events, were associated with higher PC4d levels (median [IQR] 13.6 [4.4-24.0] and 13.2 [3.2-22.3] vs. 4.0 [2.5-8.3] net MFI, respectively, p< 0.05). In a multivariable model adjusting for all significant co-variates identified in the univariable analysis (aPL, smoking, antimalarial use and prednisone >7.5mg/day), the association between all vascular events and PC4d (natural log transformed) remained significant (OR 1.7 95%CI 1.2-2.5, p=0.005).
The optimal PC4d cut-off point for vascular thromboses was identified to be 10 net MFI, with a sensitivity and specificity for venous events of 56% and 78%, and for arterial 62% and 78% (Table 1); PC4d≥10 net MFI, as compared to PC4d≥20 net MFI, resulted in a greater detection of individuals with vascular events (16/28 vs 11/28 respectively). Stratifying by aPL status, PC4d10 was associated with a history of any vascular event, with a stronger association seen in patients positive for both aPL and PC4d – OR 4.6 95% CI 1.3-16.9 for PC4d+/aPL- and OR 13.0 95% CI 3.7-46.0 for PC4d+/aPL+ as compared with PC4d-/aPL- patients (Figure 1). A thrombotic score ≥ 2 (calculated using PC4d≥10) was associated with all events (arterial and venous) – OR 3.15 [95% CI 1.21, 8.19] and with arterial thrombosis – OR 4.44 [95% CI 1.24, 15.91] (Table 2).
Conclusion: PC4d and the thrombotic score associate with thrombotic events in SLE. The 10 net MFI PC4d cutoff was optimal for identifying patients with thromboses, and more specifically arterial events. PC4d10 could function more effectively as a biomarker of cardiovascular events, providing a novel risk indicator independent of aPL antibodies.
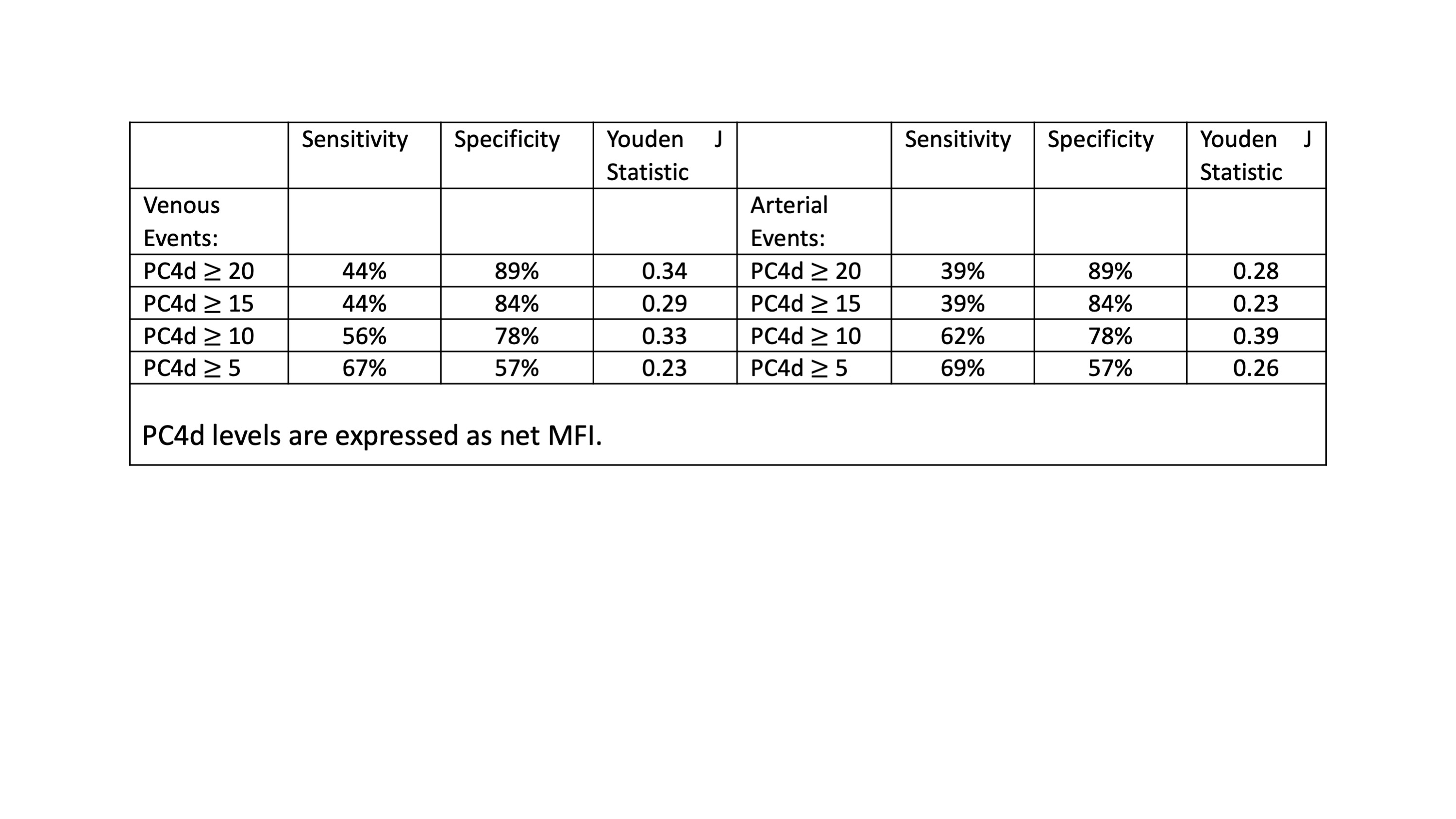 Table 1: Sensitivity and specificity of different PC4d cutoff levels for history of venous and arterial vascular events.
Table 1: Sensitivity and specificity of different PC4d cutoff levels for history of venous and arterial vascular events.
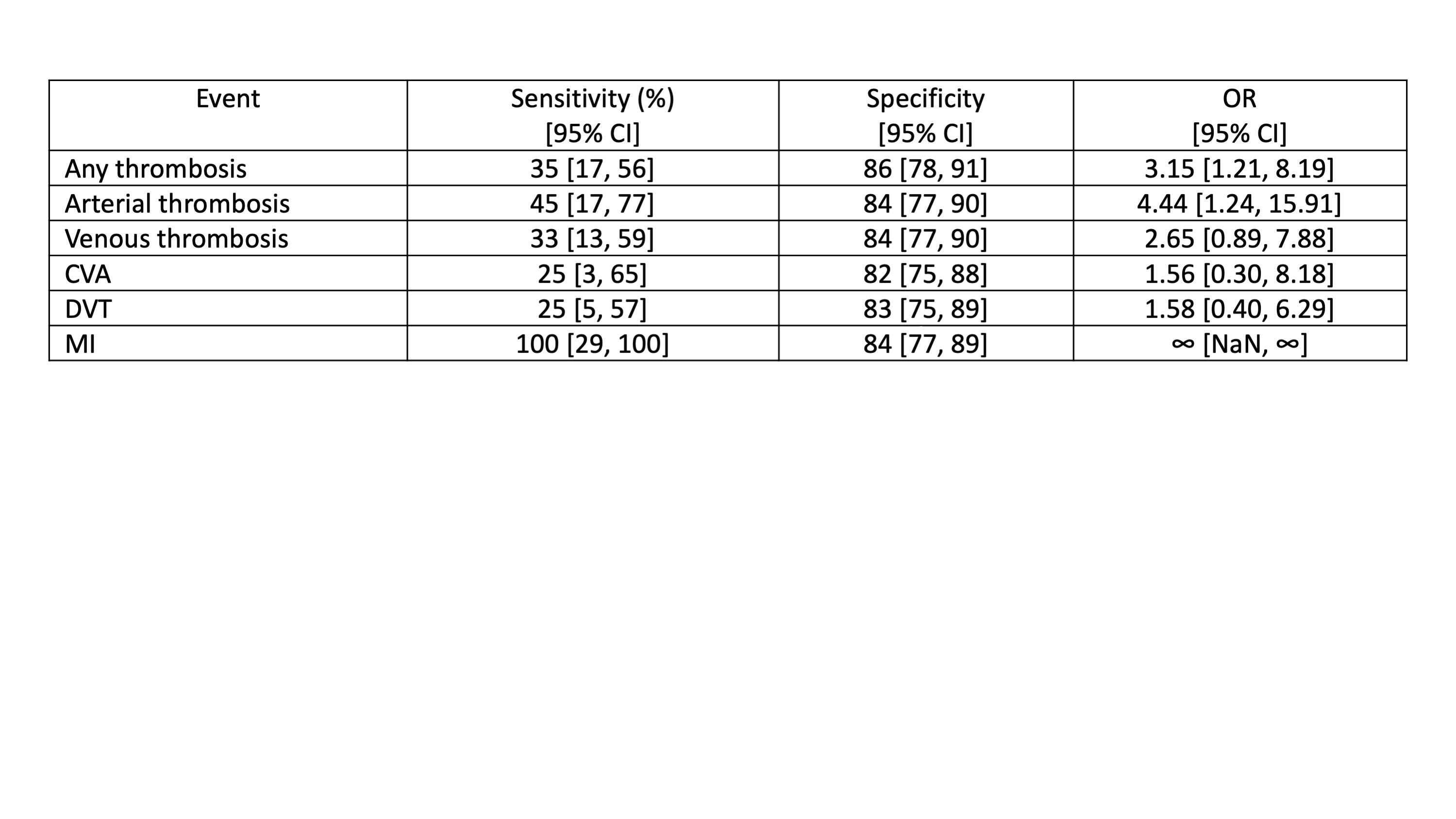 Table 2. Sensitivity, specificity, and odds ratio (OR) with 95% confidence intervals [95% CI] are reported for thrombotic score ≥ 2. The thrombotic score was calculated using cutoff for PC4d of 10 MFI. CVA: cardiovascular accidents, DVT: deep vein thrombosis, MI: myocardial infarction, NaN: not a number.
Table 2. Sensitivity, specificity, and odds ratio (OR) with 95% confidence intervals [95% CI] are reported for thrombotic score ≥ 2. The thrombotic score was calculated using cutoff for PC4d of 10 MFI. CVA: cardiovascular accidents, DVT: deep vein thrombosis, MI: myocardial infarction, NaN: not a number.
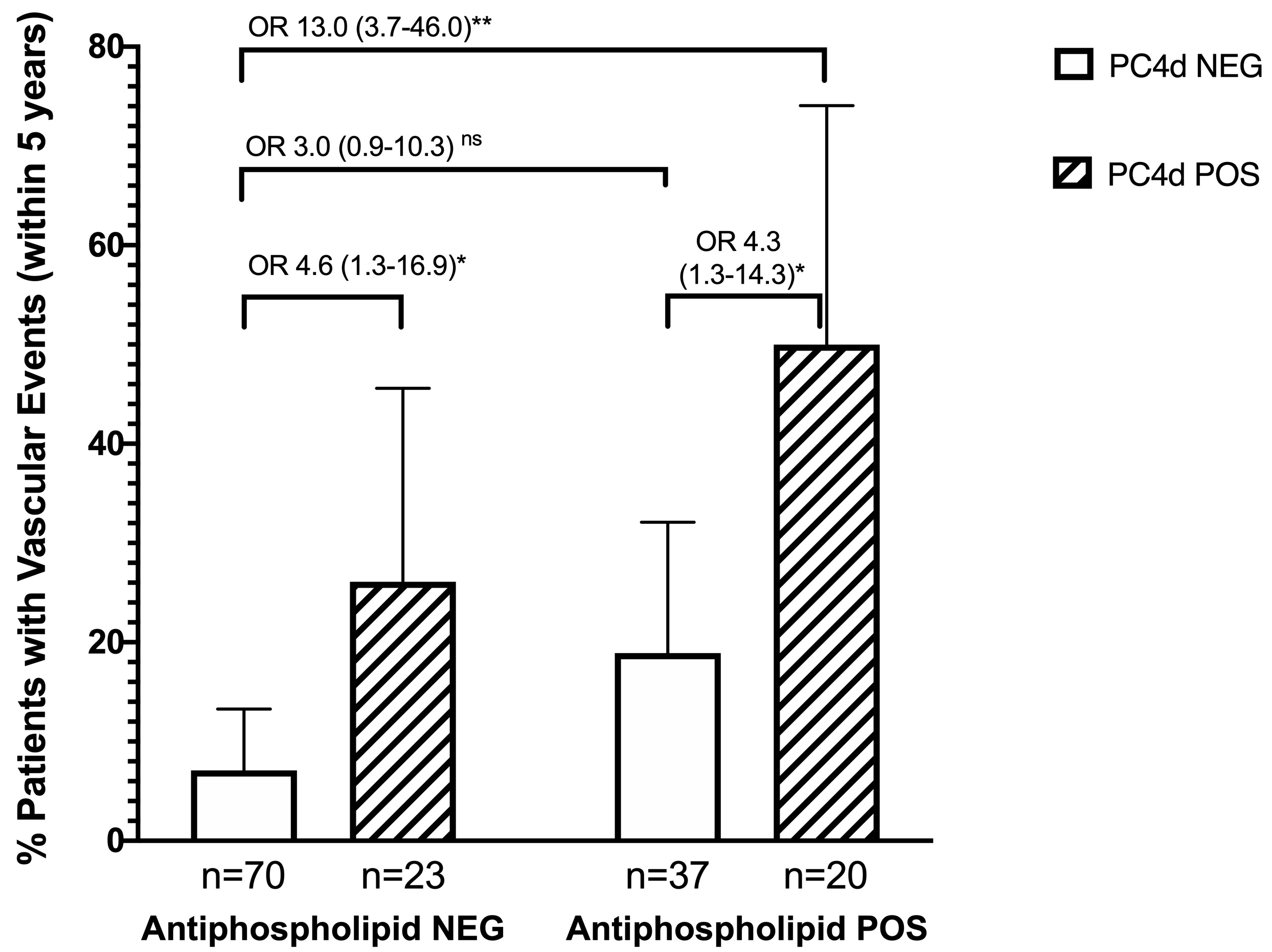 Figure 1: Vascular Events in SLE Stratified by Antiphospholipid Antibody (aPL) status and PC4d. Percent patients with a history of a vascular event within five years of study enrollment, stratified by aPL presence (NEG=negative; POS=positive) and PC4d status (NEG=PC4d 0.05.
Figure 1: Vascular Events in SLE Stratified by Antiphospholipid Antibody (aPL) status and PC4d. Percent patients with a history of a vascular event within five years of study enrollment, stratified by aPL presence (NEG=negative; POS=positive) and PC4d status (NEG=PC4d 0.05.
To cite this abstract in AMA style:
Gartshteyn Y, Alexander R, Conklin J, Dervieux T, Askanase A. Platelet-bound C4d Is Associated with an Increased Risk of Arterial and Venous Thromboses in SLE [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/platelet-bound-c4d-is-associated-with-an-increased-risk-of-arterial-and-venous-thromboses-in-sle/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/platelet-bound-c4d-is-associated-with-an-increased-risk-of-arterial-and-venous-thromboses-in-sle/
