Session Information
Date: Monday, November 8, 2021
Title: Systemic Sclerosis & Related Disorders – Clinical Poster II (1364–1390)
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Lung manifestations of systemic autoimmune diseases are a frequent cause of early death. For many patients, current treatments cannot arrest the inexorable progression to end-stage lung disease. Lung transplantation can be life-saving, but many transplant centers withhold this option from patients with systemic autoimmune diseases due to concerns that extrapulmonary manifestations and immune abnormalities could lead to additional post-transplant risks. Additional data on lung transplant experience in patients with systemic autoimmune diseases are needed to clarify risks and benefits in this population.
Methods: We conducted a retrospective cohort study of patients undergoing lung or heart-lung transplant at Stanford University between January 1, 2005 and January 1, 2020. Patients whose lung disease was attributed to a systemic autoimmune disease were identified from among this population based on ICD-9 or ICD-10 coding followed by verification that patients fulfilled classification criteria specific to their disease by medical record review. Patients were matched 1:2 to controls without autoimmune diseases according to their age, gender, year of transplantation, indication for transplantation (interstitial lung disease vs. pulmonary hypertension) and type of transplant procedure (single lung, double lung, heart-lung). We compared overall survival in those with and without autoimmune diseases using Kaplan-Meier curves by log-rank test. We used multivariable Cox proportional hazard regression to estimate the hazard ratios (HR) and 95% confidence intervals (CI) for overall survival following transplant accounting for the variables described above.
Results: In total, 75 lung or heart-lung transplant patients with systemic autoimmune diseases were identified, including 17 with rheumatoid arthritis, 16 with systemic sclerosis, 15 with sarcoidosis, 14 with idiopathic inflammatory myositis, eight with Sjogren’s syndrome, four with mixed connective tissue disease, and one with systemic lupus erythematosus. These patients were matched to 152 patients without autoimmune diseases. One-year and five-year survival was 79.4% and 54.9% in patients with autoimmune diseases and 90.3% and 57.7% in the matched cohort (p=0.16). The hazard ratio for overall survival following transplant favored patients without autoimmune diseases but was not significantly different from those with autoimmune diseases (unadjusted HR 1.29, 95% CI [0.80 – 2.08] p-value 0.31, adjusted HR 1.24, 95% CI [0.71 – 2.18] p=0.45).
Conclusion: Patients with systemic autoimmune disease fared as well after lung or heart-lung transplantation as patients without systemic causes of end-stage lung disease. These data continue to provide support for lung transplantation as a life-saving option for well-qualified patients with systemic autoimmune diseases.
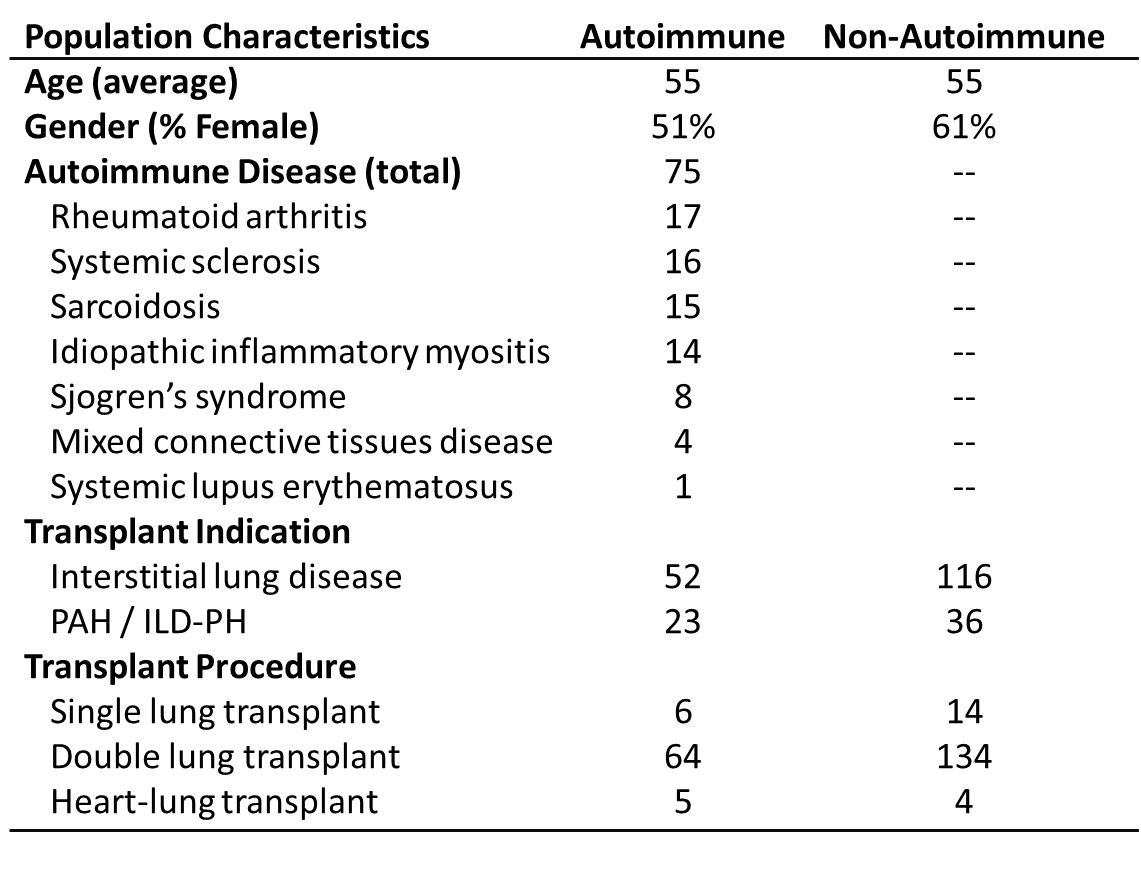 Basic population characteristics of patients who underwent lung transplantation for end-stage lung disease due to their underlying systemic autoimmune disease compared to matching patients without systemic autoimmune diseases
Basic population characteristics of patients who underwent lung transplantation for end-stage lung disease due to their underlying systemic autoimmune disease compared to matching patients without systemic autoimmune diseases
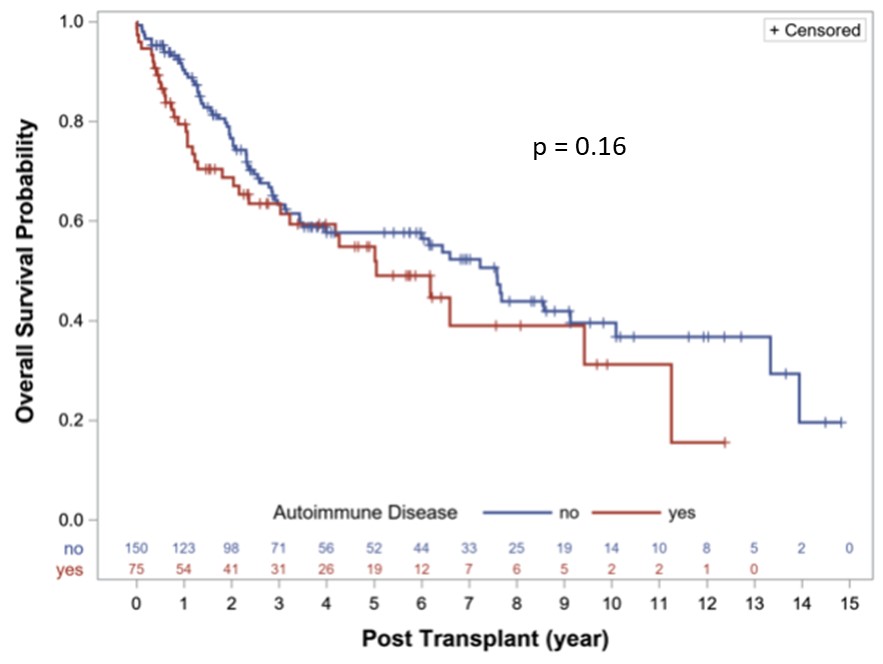 Kaplan-Meier survival curves comparing post-lung transplant survival in patients with systemic autoimmune diseases (red) versus those without (blue)
Kaplan-Meier survival curves comparing post-lung transplant survival in patients with systemic autoimmune diseases (red) versus those without (blue)
To cite this abstract in AMA style:
Melehani J, Li S, Mooney J, Chung L. Overall Survival in Patients with Systemic Autoimmune Diseases Following Lung or Heart-Lung Transplantation at a Single High-Volume Academic Transplant Center: A Comparative Cohort Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/overall-survival-in-patients-with-systemic-autoimmune-diseases-following-lung-or-heart-lung-transplantation-at-a-single-high-volume-academic-transplant-center-a-comparative-cohort-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/overall-survival-in-patients-with-systemic-autoimmune-diseases-following-lung-or-heart-lung-transplantation-at-a-single-high-volume-academic-transplant-center-a-comparative-cohort-study/
