Session Information
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Osteoarthritis (OA) is a highly prevalent disease resulting in joint pain and impaired function. Allergic pathways, including mast cell activation, may play a key role in the pathogenesis of OA.1 The association between atopic disease and the development of OA is not well understood. The objective of this study was to determine the incidence of OA in patients with atopic disease compared with the general population.
Methods: We conducted a retrospective cohort study using claims data from the Optum Clinformatics™ Data Mart and electronic health record data from the Stanford Research Repository (STARR). We included adult patients with more than 5 years of continuous enrollment and excluded patients with preexisting OA or a history of inflammatory arthritis. The exposed group included patients with a diagnosis of incident atopic disease, including asthma and atopic dermatitis. The control group included patients without atopic disease. The primary outcome was the development of OA, defined as two or more ICD-9 or -10 codes for OA separated by seven days or more. In the Optum cohort, the relationship between atopic disease and the development of OA was evaluated using logistic regression, adjusting for age, sex, race/ethnicity, Charlson comorbidity score, education, duration of follow-up, and frequency of outpatient visits. In the STARR cohort, we additionally adjusted for body mass index (BMI), and we were unable to adjust for education.
Results: The Optum cohort included 35,097 patients with asthma, 77,854 patients with atopic dermatitis, 4,395 patients with both asthma and atopic dermatitis, and 2,242,901 control patients without atopic disease (Table 1). The STARR cohort included 11,101 patients with asthma, 23,855 patients with atopic dermatitis, 8,773 patients with both asthma and atopic dermatitis, and 70,705 control patients without atopic disease (Table 2). There was a higher incidence of OA in patients with asthma (24.7% in Optum; 17.6% in STARR), atopic dermatitis (20.2% in Optum; 15.4% in STARR), and both asthma and atopic dermatitis (32.0% in Optum; 15.2% in STARR) compared to non-atopic control patients (13.7% in Optum; 8.9% in STARR) (Table 3). In the Optum cohort, there was an 84% increased risk of developing OA for patients with both asthma and atopic disease compared to non-atopic control patients (adjusted odds ratio (OR) 1.84; 95% CI, 1.71-1.97; p< .001) (Table 3). In the STARR cohort, after additionally adjusting for BMI, there was a similarly increased risk of OA in patients with both asthma and atopic dermatitis compared to controls, with an adjusted OR of 1.54 (95% CI, 1.44-1.65; p< 0.001) (Table 3).
Conclusion: This study demonstrates an increased incidence of OA in patients with atopic disease compared to the general population. The association between atopic disease and OA is supported by recent observations that mast cells and type II cytokines play important roles in the pathogenesis of OA. Our findings provide further evidence that allergic pathways may contribute to the development of OA, and future interventional studies could consider targeting these pathways for the treatment of OA.
References:
1. Wang Q, Lepus CM, Raghu H, et al., Elife 8, (2019).
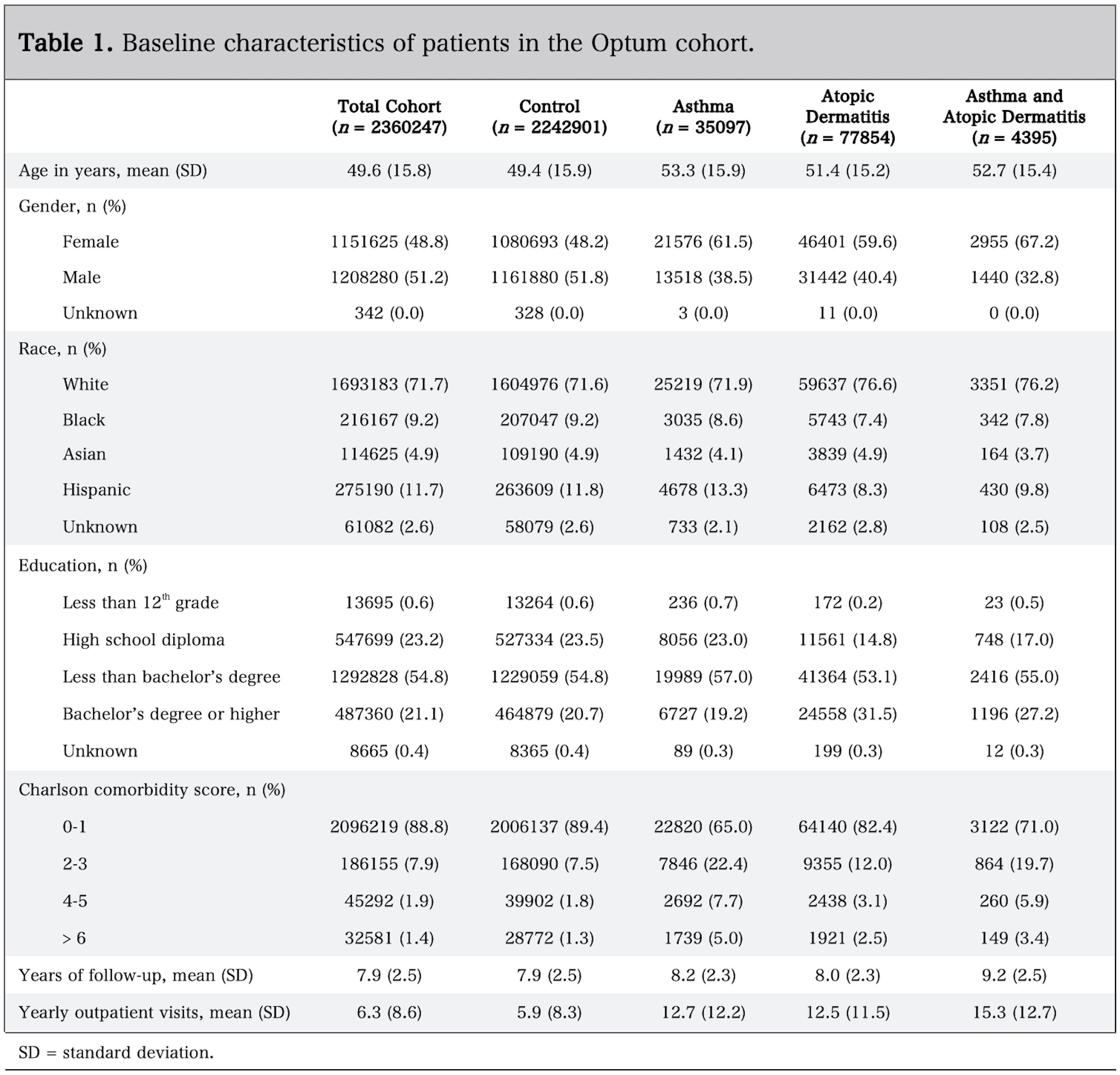 Table 1. Baseline characteristics of patients in the Optum cohort.
Table 1. Baseline characteristics of patients in the Optum cohort.
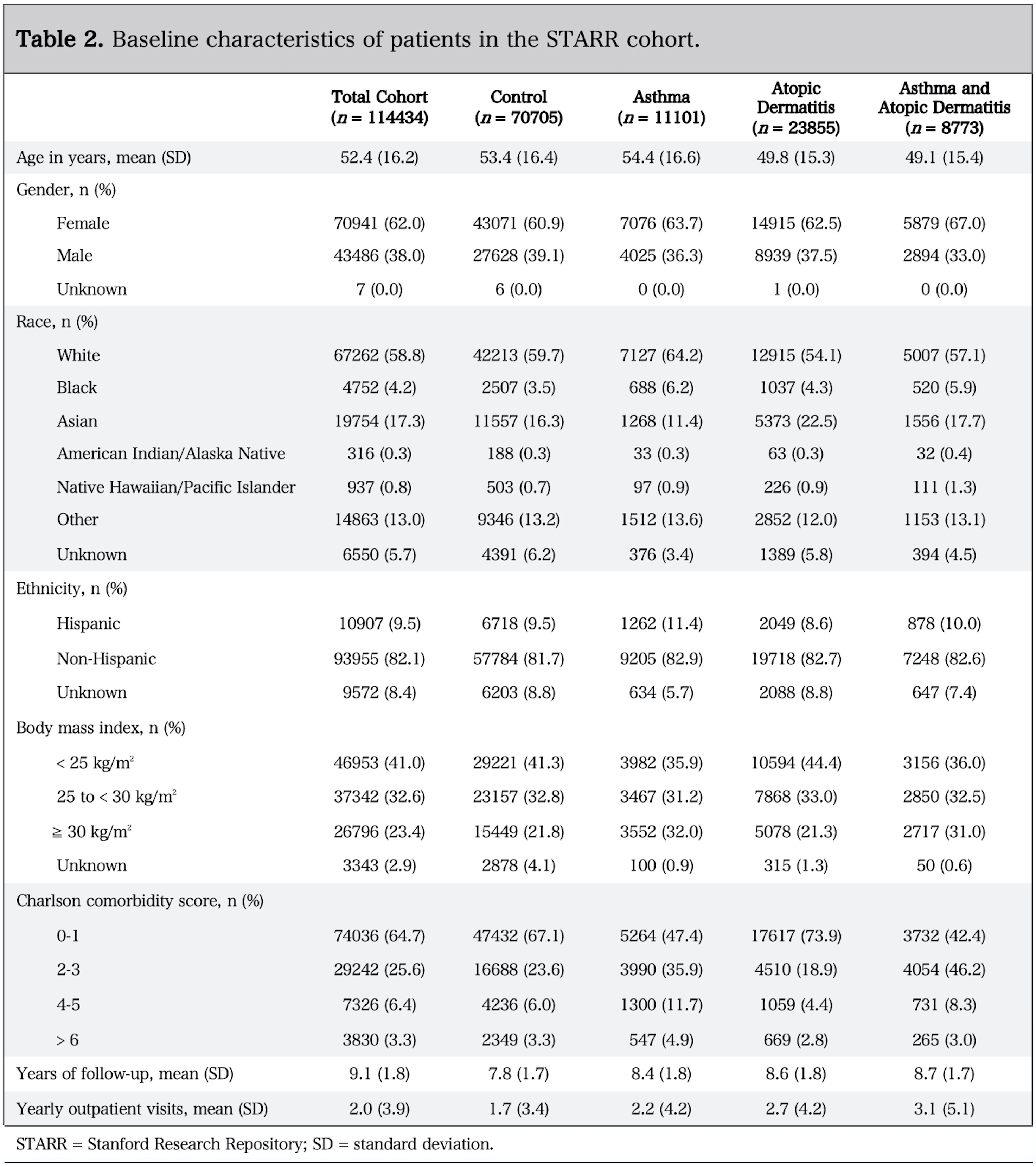 Table 2. Baseline characteristics of patients in the STARR cohort.
Table 2. Baseline characteristics of patients in the STARR cohort.
 Table 3. Incidence of osteoarthritis in patients with atopic disease compared to non-atopic control patients.
Table 3. Incidence of osteoarthritis in patients with atopic disease compared to non-atopic control patients.
To cite this abstract in AMA style:
Baker M, Sheth K, Lu R, Lu D, von Kaeppler E, Bhat A, Felson D, Robinson W. Osteoarthritis Risk Is Increased in Patients with Atopic Disease [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/osteoarthritis-risk-is-increased-in-patients-with-atopic-disease/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoarthritis-risk-is-increased-in-patients-with-atopic-disease/
