Session Information
Date: Saturday, November 16, 2024
Title: Abstracts: Osteoarthritis – Novel Insights from Observational Studies
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: People with knee osteoarthritis (OA) and obesity (i.e. BMI ≥30kg/m2) have poorer function than those without obesity. However, function is not uniform among people with obesity. It is possible that those with concurrent low muscle mass [i.e. sarcopenic obesity (SO)], or metabolic-related comorbidities but without low muscle [i.e. clinical comorbid obesity (CCO)] may have worse functional outcomes than those without either [i.e. uncomplicated or normal obesity (NO)]. Understanding if these distinct obesity subtypes contribute differentially to patterns of functional deterioration is needed to support targeted OA prevention and treatment strategies. We examined the relationship between obesity subtypes and trajectories of functional change after a 7-year follow-up period.
Methods: Participants from the Multicenter Osteoarthritis Study (MOST), a NIH-funded longitudinal cohort of individuals with or at-risk for knee OA, with a BMI ≥30 kg/m2 and baseline body composition data from DXA were included. The SO group had low muscle mass [appendicular lean soft tissue adjusted for weight] and high percent fat mass, defined by age and sex-specific cutpoints. The CCO group had metabolic comorbidities [self-reported diabetes, heart, liver, or pulmonary disease from the Charlson Comorbidity Index] but no low muscle. The NO group met neither SO or CCO definitions. Self-reported physical functioning was measured with WOMAC. Longitudinal patterns of physical function over 7-years were identified using a group-based trajectory model, with best-fit determined by low BIC and AIC, and high posterior probability of group membership. The relationship between obesity subtypes and trajectory group membership was examined using multinomial logistic regression.
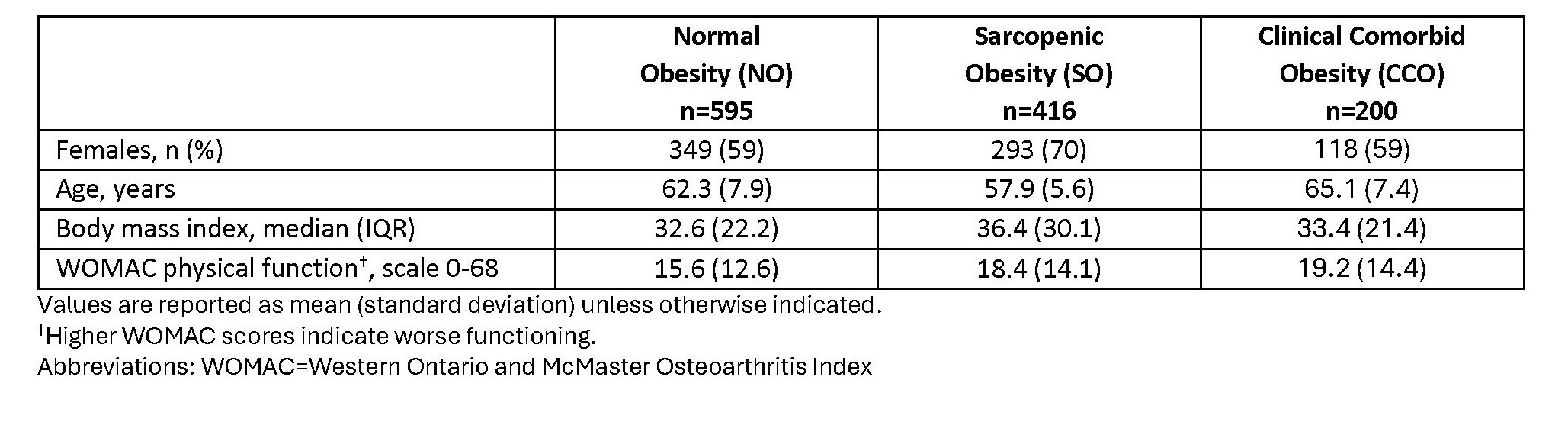
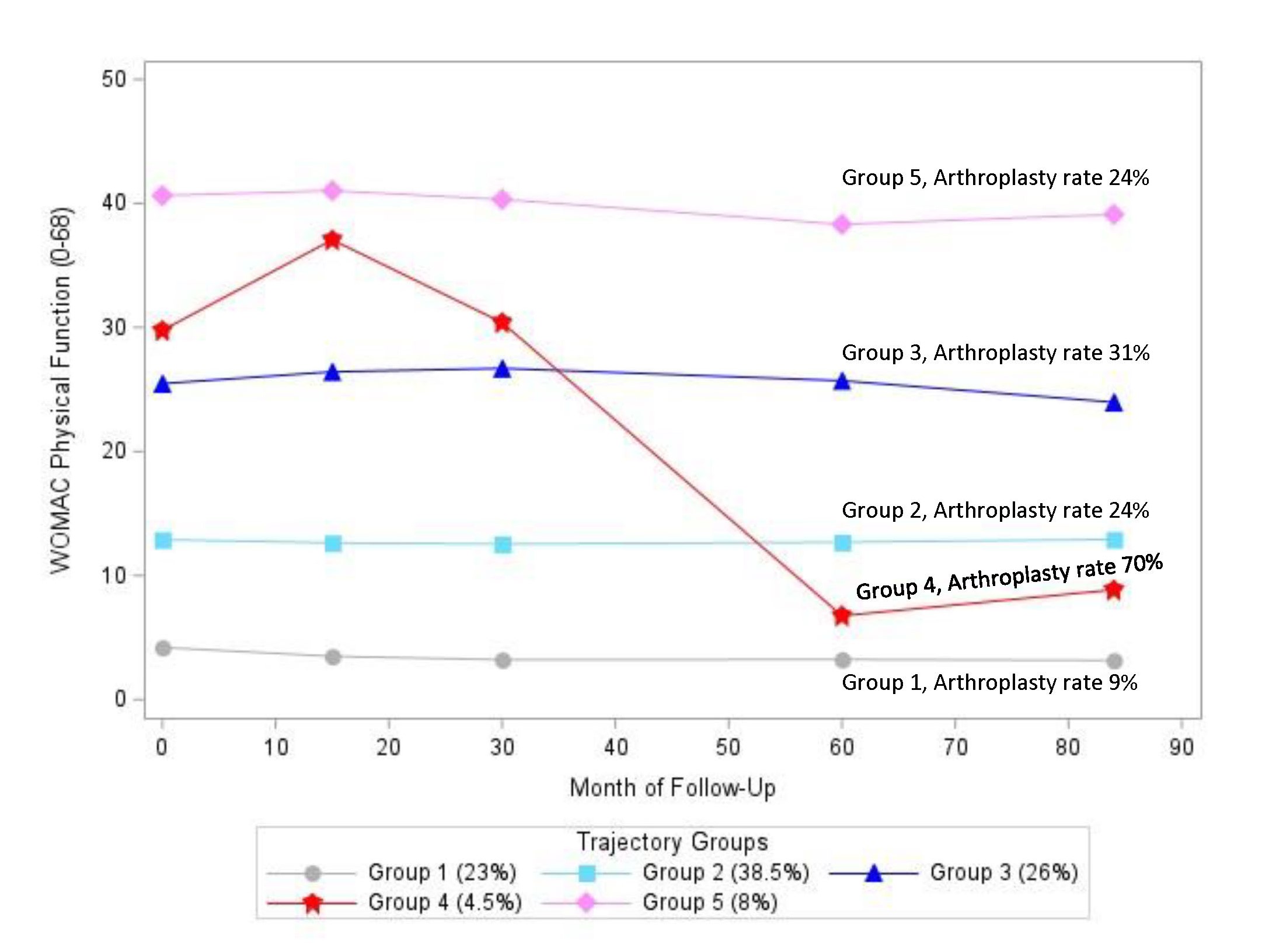
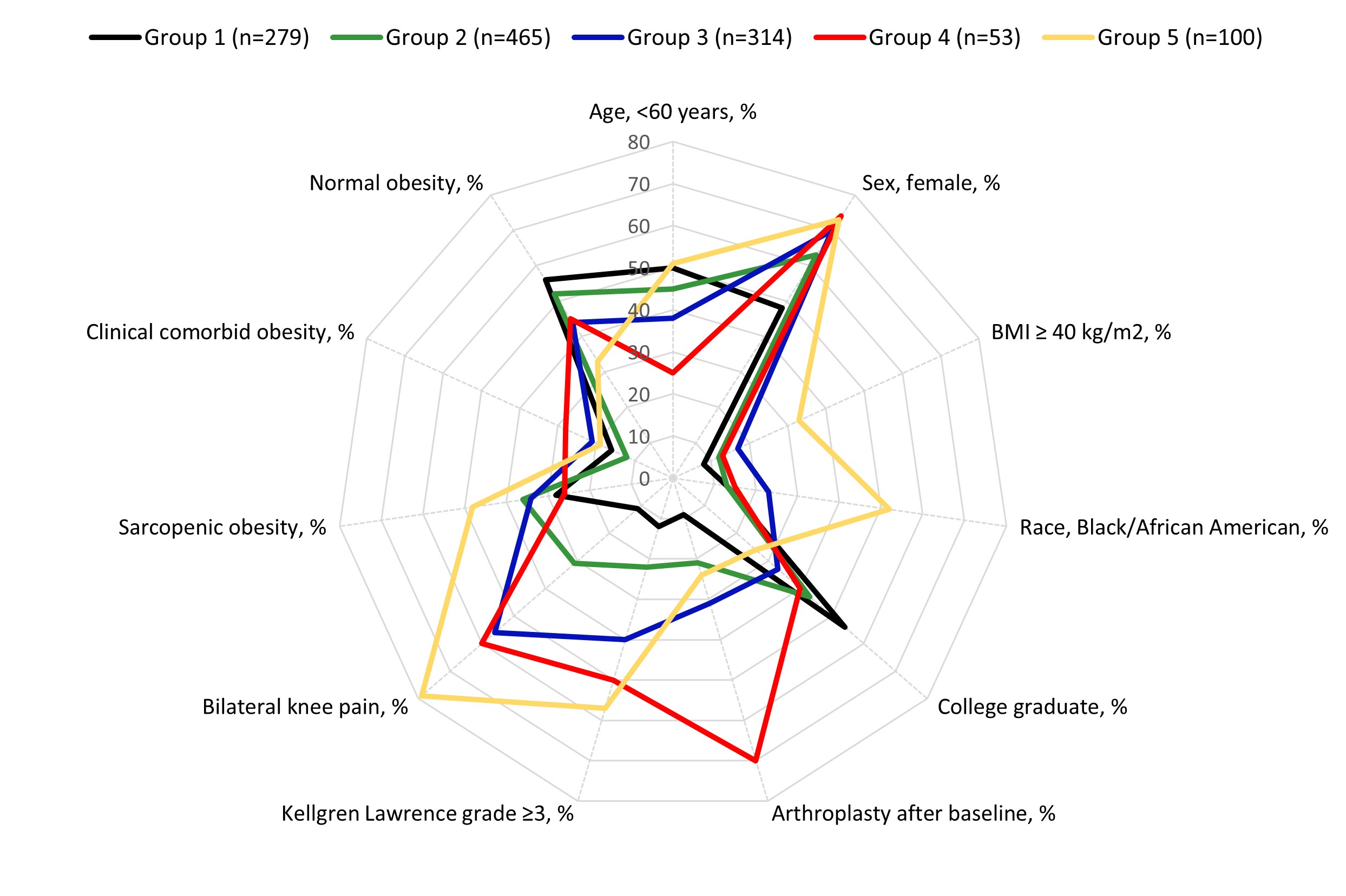
Results: We included 1211 individuals (63% female, mean age 61.2±7.6 years, BMI 35.0±4.5 kg/m2). Compared to the NO group, both SO and CCO groups had worse physical function at baseline (Table 1). We identified 5 trajectories (TRAJ) of functional change over 7-years (Figure 1). Four of the five TRAJ reflected stable but distinct levels of functioning across 7-years, with TRAJ 3 and 5 having persistent poorer function. One group (TRAJ 4) demonstrated an improvement in WOMAC function during follow-up; group members were older and had higher rates of arthroplasty over follow-up than other TRAJ groups (Figure 2). A greater proportion of individuals in the persistent poorer function trajectory groups (TRAJ 3 and 5) were Black, had lower rates of post-secondary education, and higher rates of severe knee OA and a BMI ≥40 kg/m2 (Figure 2). The CCO group had higher odds of being in TRAJ 3, 4, and 5 [OR 2.1, 2.8, 2.5, respectively] than TRAJ 2 compared with the NO group. The SO group had higher odds of being in TRAJ 5 [OR 2.1], the worst function group.
Conclusion: Individuals with obesity and concurrent low muscle mass or metabolic comorbidities have persistent, worse impairments in functional status over a 7-year period compared to those with obesity alone. Distinguishing these obesity subtypes through body composition and comorbidity assessments may be needed to enable personalized intervention and to avoid extended mobility disability.
To cite this abstract in AMA style:
Godziuk K, Tilley S, LaValley m, Nevitt M, Lewis C, Torner J, Neogi T. Obesity Subtypes and Trajectories of Functional Change After 7-years of Follow-up: The Multicenter Osteoarthritis (MOST) Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/obesity-subtypes-and-trajectories-of-functional-change-after-7-years-of-follow-up-the-multicenter-osteoarthritis-most-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/obesity-subtypes-and-trajectories-of-functional-change-after-7-years-of-follow-up-the-multicenter-osteoarthritis-most-study/