Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Baseline high Neutrophil- to- lymphocyte ratio (NLR) (higher than 2.95) is associated with severe progressive skin and lung disease and with reduced 5-year survival in systemic sclerosis (SSc). It is not known whether NLR changes in response to treatment. The aim of our study was to evaluate NLR changes as a biomarker for treatment response in SSc.
Methods: Progressive SSc patients who were treated with autologous hematopoietic stem cell transplantation (AHSCT), combination therapy of rituximab and mycophenolate mofetil or chimeric antigen receptor (CAR-T) therapy were recruited, along with healthy controls (HC). Clinical improvement (CI) at 12 months was defined as a decrease in modified Rodnan Skin Score (mRSS) by more than 25% or an increase in forced vital capacity (FVC) by more than 10%. Event-free survival (EFS) was defined survival without persistent major organ failure (heart, lung, kidney) at 12 months.NLR, mRSS and FVC were repeatedly assessed.
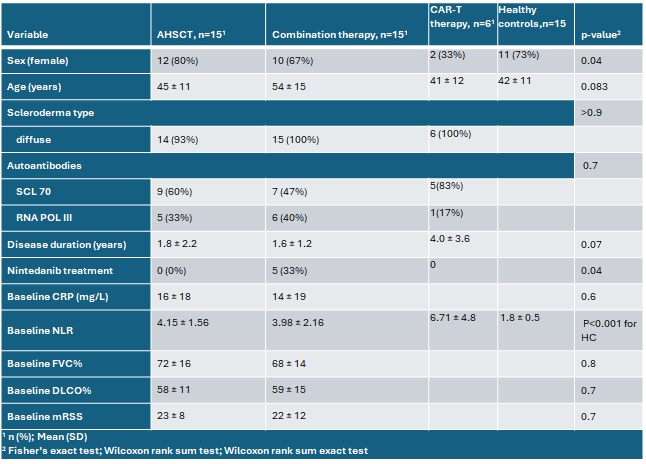
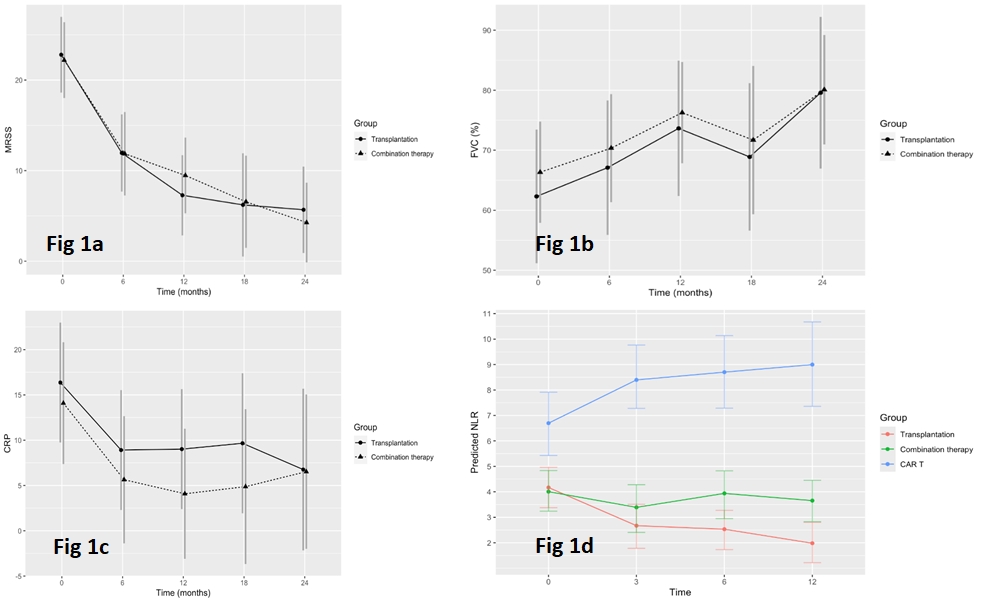
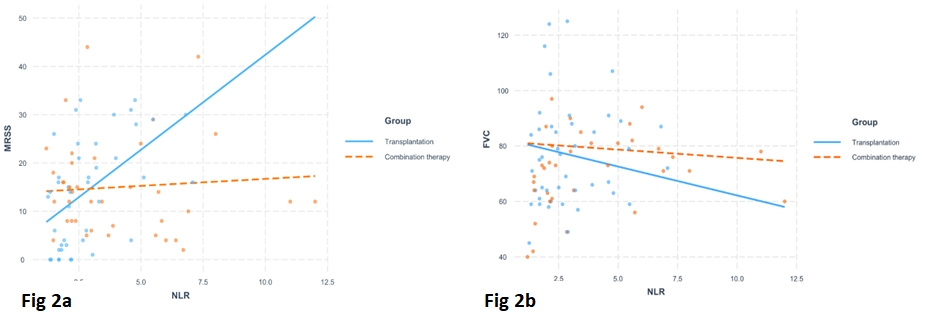
Results: Fifteen patients were recruited in the AHSCT, combination therapy and HC groups and 6 in the CAR-T group. Clinical characteristics were similar, but for lower rate of women in the CAR T group (table 1). Baseline mean NLR was high ( >2.95) in all treatment arms: AHSCT, combination therapy and CAR-T, compared to HC (1.8±0.5), p< 0.001 (table 1). CI was similar between groups, 93% (14/15) in the AHSCT, 100% (15/15) in the combination group and (100%) in the CAR-T group. EFS was similar as well, 100% (15/15) in the AHSCT group, 93% (14/15) in the combination group and 100% for the CAR T (p=NS). A similar and statistically significant decrease in mRSS values and increase in FVC% was evident after AHSCT and in combination group at each time point up to 12 months in a linear mixed model (fig. 1a-b). Despite similar clinical response and similar decrease in CRP levels (fig. 1c), NLR decreased significantly at all timepoints only after AHSCT from 4.15±1.56 to 1.8±0.4 (fig1d) and was significantly lower compared to other groups at all time points from 3 months to 12 months, in a linear mixed model, p = 0.03. NLR correlated with mRSS and FVC only in the AHSCT group (Fig. 2a-b). After a decrease in NLR (< 2) with clinical response, NLR increased above 3 in 2 patients who had a relapse after AHSCT, one with myocarditis and renal crisis and the other with lung fibrosis.
Conclusion: High baseline NLR decreases only after AHSCT in parallel with clinical response and in correlation with mRSS and FVC. NLR may be a simple biomarker that may reflect molecular changes that occur after AHSCT but not with other therapies. Further research should evaluate NLR as a possible biomarker to define remission and diagnose a relapse after AHSCT.
Figure 1b- Forced vital capacity (FVC) % predicted. FVC was lower compared to baseline in AHSCT group and in combination therapy group at each time point compared to baseline (p<0.05).
Figure 1c- CRP was lower compared to baseline in AHSCT group and in combination therapy group at each time point compared to baseline (p<0.05).
Figure 1d- Neutrophils to lymphocytes ratio (NLR) decreased only after AHSCT and was significantly lower compared to other groups at all time points from 3 months to 12 months, in a linear mixed model, p = 0.03.
Figure 2b – Correlation between FVC% predicted and NLR- There was a negative significant correlation between FVC% predicted and NLR. For each increase of 1 unit in NLR there is decrease of _2.59 in FVC% predicted according to the NLR effect plot (p<0.03).
To cite this abstract in AMA style:
keret s, Kaly L, Schett G, Bergmann C, Henes J, Slobodin G, Rimar D. Neutrophil-to- lymphocyte Ratio: A Possible Biomarker for Clinical Response After Autologous Hematopoietic Stem Cell Transplantation [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-a-possible-biomarker-for-clinical-response-after-autologous-hematopoietic-stem-cell-transplantation/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neutrophil-to-lymphocyte-ratio-a-possible-biomarker-for-clinical-response-after-autologous-hematopoietic-stem-cell-transplantation/