Session Information
Date: Monday, October 27, 2025
Title: (1191–1220) Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Juvenile dermatomyositis (JDM) is an inflammatory vasculopathy characterized by muscle weakness and systemic inflammation. This study aimed to investigate the clinical utility of neutrophil activation markers, specifically calprotectin (S100A8/A9) and myeloperoxidase (MPO)-DNA complexes, as potential biomarkers for muscle inflammation and predictors of long-term outcomes in JDM.
Methods: Plasma levels of calprotectin and MPO-DNA were quantified using ELISA in JDM (n = 36), juvenile idiopathic arthritis (JIA, n = 13), and healthy controls (HCs, n = 21). Disease severity and muscle function were assessed using the Childhood Myositis Assessment Scale (CMAS), Physician Global Assessment (PGA), and Manual Muscle Testing 8 (MMT8).
Results: JDM patients exhibited significantly higher plasma calprotectin and MPO-DNA levels as compared to HCs (p=0.0008 and p=0.0048, respectively) (Figures 1A-B). Calprotectin levels correlated with muscle function scores (CMAS r=-0.682, p=0.0002; MMT8 r=-0.59, p=0.005; and PGA muscle scores r=0.452, p=0.014) (Figure 1C). ROC analysis demonstrated that baseline calprotectin and MPO-DNA levels could distinguish active disease with high accuracy (AUC = 0.85 and 0.80, respectively) (Figure 1D). Further stratification showed that patients with elevated levels of both markers had significantly worse disease activity and muscle involvement (Figures 1E-F). Notably, higher baseline levels of these markers correlated with improved MMT8 scores over time (r=0.634, p=0.027; r=0.582, p=0.047) (Figures 2A-B), indicating a predictive role in muscle recovery.
Conclusion: Calprotectin and MPO-DNA represent promising biomarkers for muscle inflammation and functional outcomes in JDM. These results suggest that neutrophil activation plays a key role in JDM pathogenesis and may provide insights into disease monitoring and treatment strategies.
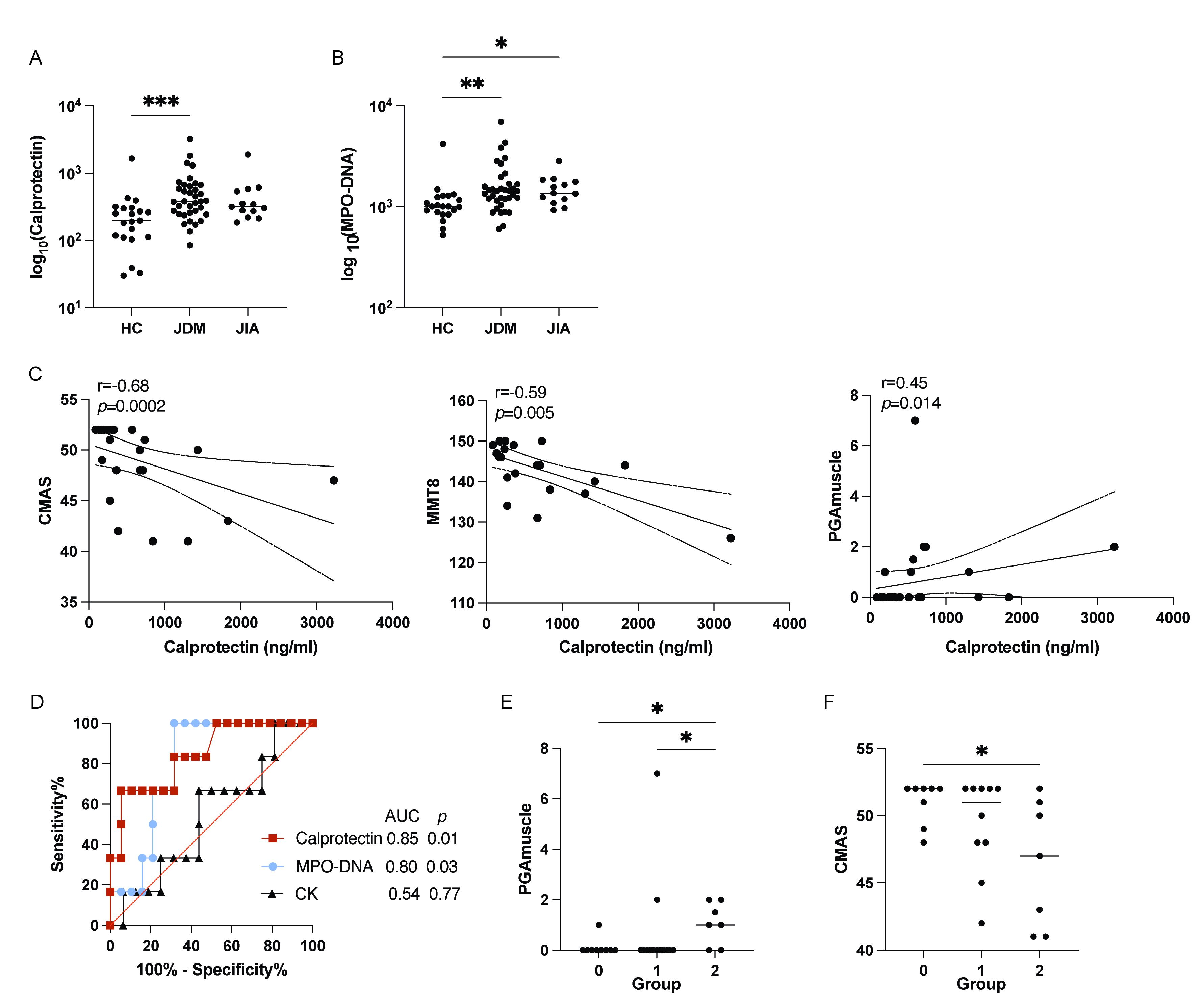 Figure 1. Neutrophil activation levels in JDM and associations with disease activity markers. (A, B) Levels of calprotectin (A) and MPO-DNA (B) in plasma among different groups. (C) Correlation of calprotectin with CMAS, MMT8, and PGA muscle score. (D) ROC curves comparing the performance of calprotectin, MPO-DNA and CK levels in distinguishing active from remission states in JDM patients based on CMAS. Active disease was defined as a CMAS ≤ 47. (E-F) PGA muscle scores (E) and CMAS (F) in JDM patients stratified into three groups based on neutrophil activation marker levels. Group 0: low level of both calprotectin and MPO-DNA; Group 1: elevated level of either biomarker; Group 2: elevated levels of both biomarkers.
Figure 1. Neutrophil activation levels in JDM and associations with disease activity markers. (A, B) Levels of calprotectin (A) and MPO-DNA (B) in plasma among different groups. (C) Correlation of calprotectin with CMAS, MMT8, and PGA muscle score. (D) ROC curves comparing the performance of calprotectin, MPO-DNA and CK levels in distinguishing active from remission states in JDM patients based on CMAS. Active disease was defined as a CMAS ≤ 47. (E-F) PGA muscle scores (E) and CMAS (F) in JDM patients stratified into three groups based on neutrophil activation marker levels. Group 0: low level of both calprotectin and MPO-DNA; Group 1: elevated level of either biomarker; Group 2: elevated levels of both biomarkers.
Statistical analyses by Kruskal-Wallis test, Spearman correlation and Mann-Whitney U test with * p < 0.05, ** p < 0.01, and *** p < 0.001.
.jpg) Figure 2. Correlations of neutrophil activation markers and disease progression in JDM. (A-B) Correlation analysis between plasma levels of calprotectin (A) and MPO-DNA (B) and MMT8 progression in JDM.
Figure 2. Correlations of neutrophil activation markers and disease progression in JDM. (A-B) Correlation analysis between plasma levels of calprotectin (A) and MPO-DNA (B) and MMT8 progression in JDM.
Statistical analyses by Spearman correlation.
To cite this abstract in AMA style:
Shi J, Wu Y, Levy A, Wang T, Janappareddi A, Hermanson P, Gonzalez-Chapa J, Wang Q, Shenoi S, Lood C. Neutrophil Activation in Juvenile Dermatomyositis: Associations with Muscle Function and Disease Progression [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/neutrophil-activation-in-juvenile-dermatomyositis-associations-with-muscle-function-and-disease-progression/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neutrophil-activation-in-juvenile-dermatomyositis-associations-with-muscle-function-and-disease-progression/
