Session Information
Date: Monday, November 13, 2023
Title: (1013–1032) Healthcare Disparities in Rheumatology Poster II: Socioeconomic Determinants
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite the proven cardioprotective benefits of statin therapy in RA, concern for statin-associated muscle symptoms (SAMS) might deter clinicians from prescribing them to DM/PM patients with Hyperlipidemia (HLD), particularly those with disease-derived myopathy. This analysis aims to quantify and compare the initiation rates of statin therapy in patients with RA-HLD and DM/PM-HLD, with a focus on whether a diagnosis of DM/PM leads to the underutilization of these drugs.
Methods: Utilizing the TriNetX Research Network, we analyzed de-identified electronic health records from U.S.-based entities over the last five years. Inclusion criteria required the HLD diagnosis to follow the initial RA or DM/PM diagnosis by one day to five years. All patients included were on immunosuppressive medications, and we excluded patients with a second autoimmune disease diagnosis or on treatment with lipid-lowering medications other than statins. The detection of NormRx code for HMG CoA reductase inhibitors identified statin initiation. The analysis considered the HLD diagnosis (Index Event) point following RA or DM/PM diagnosis and the succeeding one month to five years (Time Window). Propensity score matching was employed for age, race, sex, ethnicity, cardiovascular risk factors, and cardiovascular diseases. TriNetX software aided in cohort matching and statistical computations. The measure of association was the Risk Ratio of statin initiation post the Index Event. A confidence interval of 95% was used, with a significance level of p < 0.05 (2-sided).
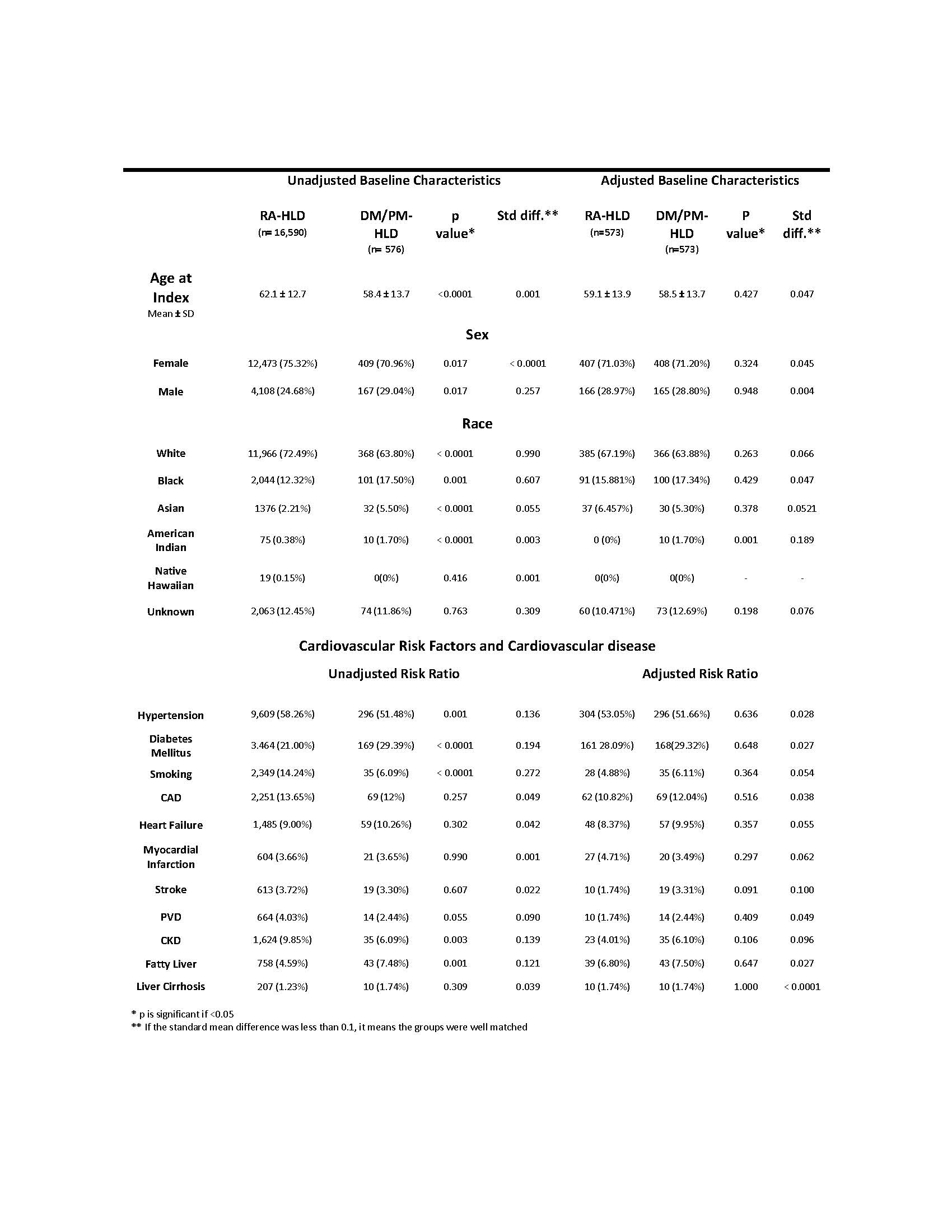
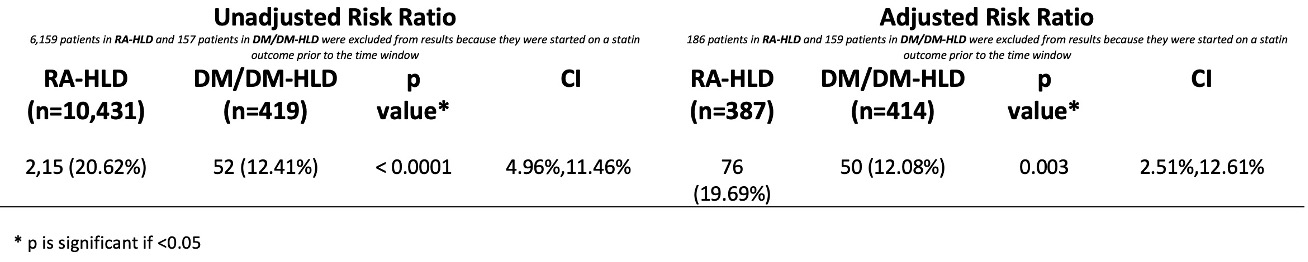
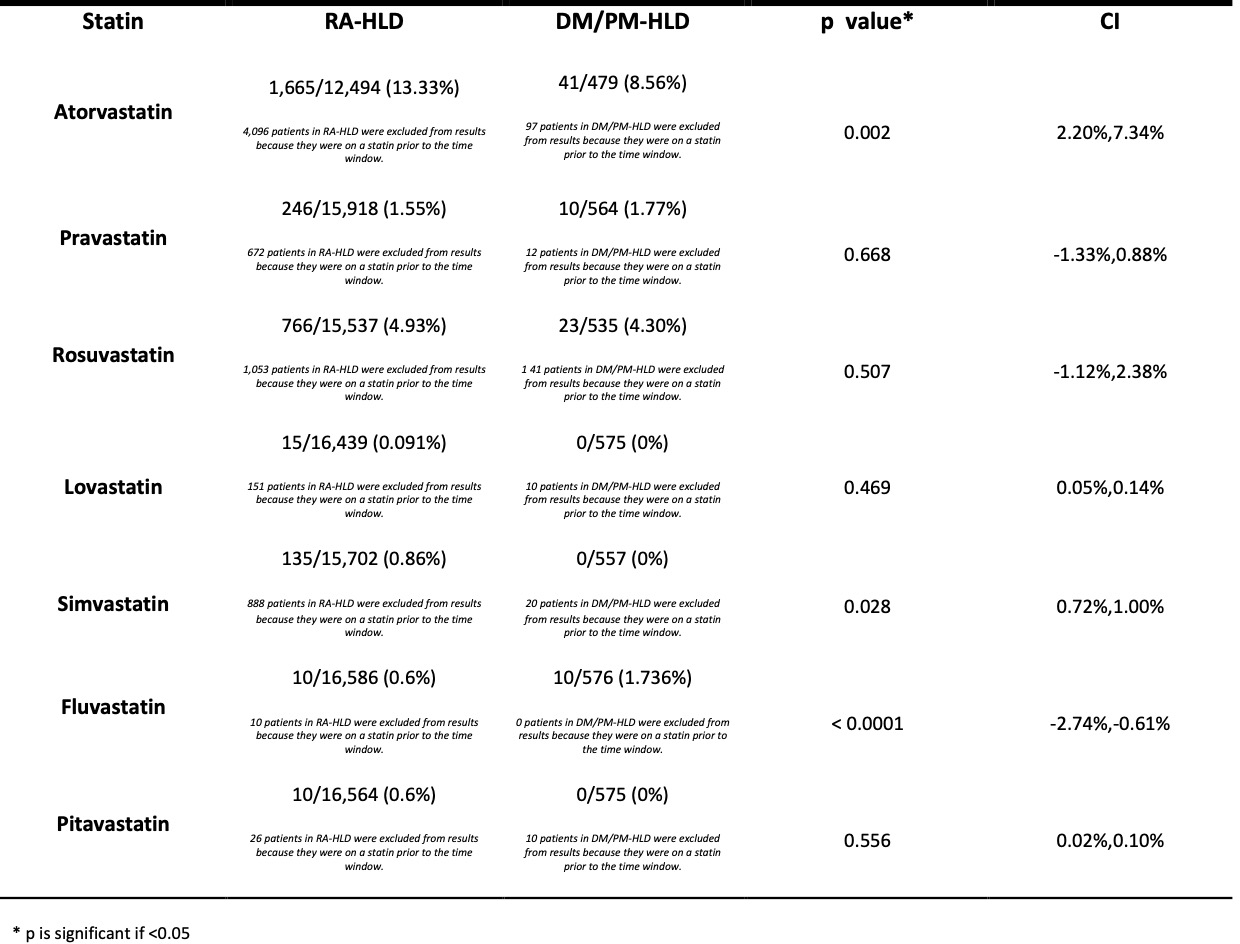
Results: The study included 16,590 RA-HLD and 576 DM/PM-HLD patients from 2018-2023, with average ages at HLD diagnosis being 62 (RA-HLD) and 58 (DM/PM-HLD). Both groups were predominately female and of White race (75% RA-HLD and 71% DM/PM-HLD), with a higher proportion of Black and Asian patients in the DM/PM-HLD cohort (Table 1). Statin initiation therapy was significantly higher among the RA-HLD cohort (20.6%) compared to the DM/PM-HLD cohort (12.4%) [CI 4.96%,11.46%, p < 0.0001], excluding those already on statin therapy. This trend persisted even with propensity score matching, with initiation rates of 19.6% for the RA-HLD groups and 12%, for the DM/PM-HLD groups [CI 2.51%, 12.61%, p 0.003] (Table 2). Regarding specific statin therapy, Atorvastatin was more commonly detected in the RA-HLD group (13% vs 8.5%), while Fluvastatin was more prevalent in the DM/PM-HLD cohort (1.73% vs 0.6%). Notably, Simvastatin nor Pitavastatin were not detected to DM/PM-HLD patients, whereas rates of Pravastatin, Rosuvastatin, and Lovastatin were similar among both groups (Table 3).
Conclusion: Despite the inherent limitations of an electronic health records-based database this study shows a concerning signal of disparity in statin initiation rates in DM/PM-HLD compared to RA-HLD patients. These results emphasize the urgent need for improved cardiovascular disease risk assessment and the development of guidelines for targeting DM/PM-HLD patients. Future research should explore factors contributing to this under-treatment and evaluate the potential risks and benefits of utilizing statins in this unique patient population.
To cite this abstract in AMA style:
Fares J, Summer r, Loizidis G. Lower Rates of Statin Therapy Initiation in Dermatomyositis/Polymyositis vs. Rheumatoid Arthritis Patients with Hyperlipidemia: A Multicenter USA-Based Study (2018-2023) [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/lower-rates-of-statin-therapy-initiation-in-dermatomyositis-polymyositis-vs-rheumatoid-arthritis-patients-with-hyperlipidemia-a-multicenter-usa-based-study-2018-2023/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lower-rates-of-statin-therapy-initiation-in-dermatomyositis-polymyositis-vs-rheumatoid-arthritis-patients-with-hyperlipidemia-a-multicenter-usa-based-study-2018-2023/