Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In developing algorithms within claims databases that may inform how to find patients with psoriatic arthritis (PsA) prior to diagnosis, it is important to identify meaningful potential predictors that appear prior to diagnosis. This study aims to better understand PsA patient pathways by examining the sequences of health events over the 6 years prior to PsA diagnosis, as well as differences in patients with and without PsA.
Methods: This retrospective cohort study used administrative claims data from patients in the Truven Health MarketScan® Commercial and Medicare Supplemental Databases from January 2006 to April 2019. The PsA population included all patients aged ≥ 18 years with ≥ 2 diagnoses of PsA (ICD-9-CM/ICD-10-CM) ≥ 30 days apart who had ≥ 6 years of continuous enrollment prior to first PsA diagnosis. Control (non-PsA) patients were matched 2:1 to patients with PsA by age, sex, geographic location, insurance, and enrollment duration. Sequences of health events as described by diagnosis codes, procedures performed, drugs prescribed, and physician types were examined over the 6 years prior to PsA diagnosis and for controls; results were also stratified by psoriasis vs no psoriasis prior to PsA diagnosis.
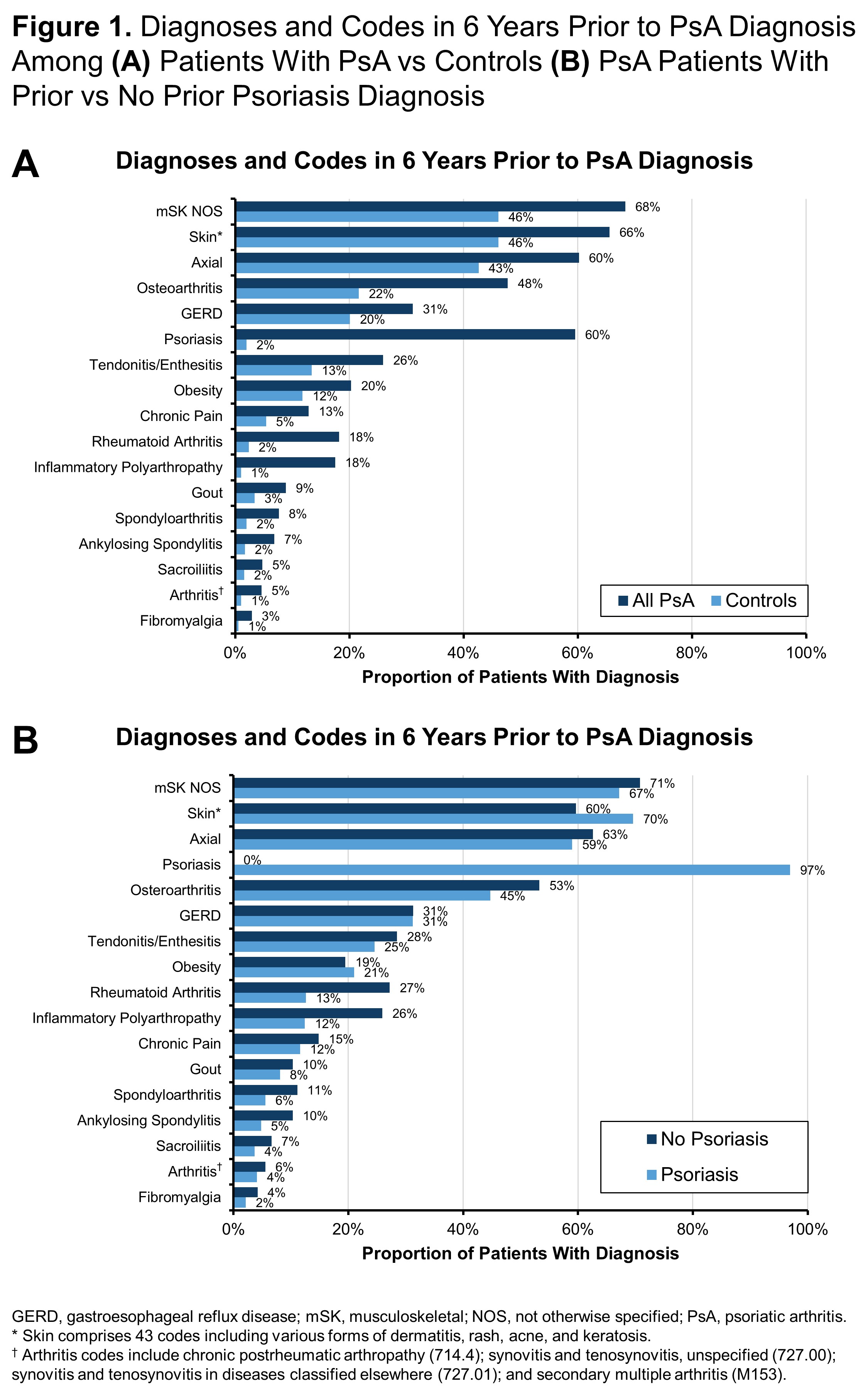
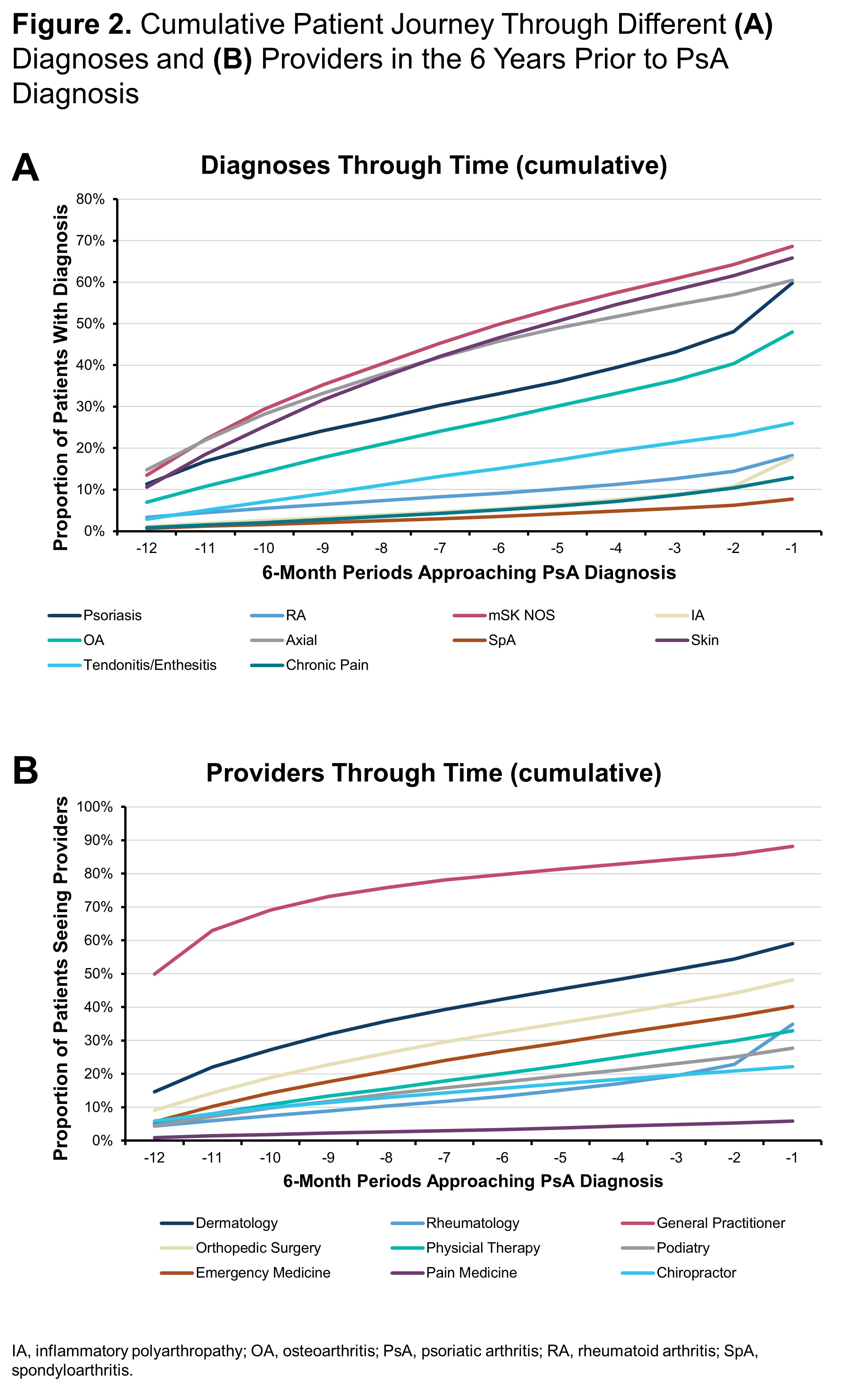
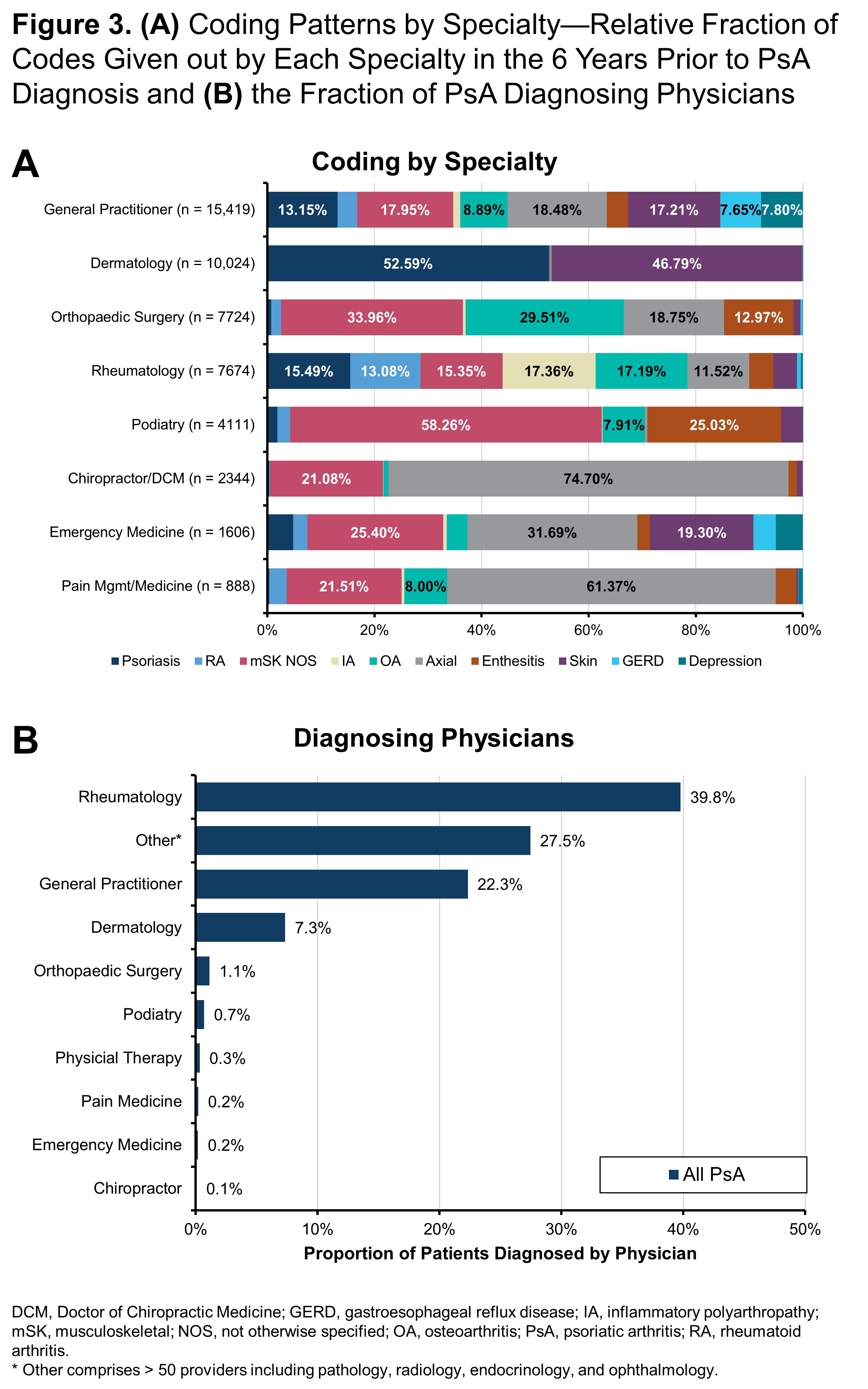
Results: Among 13,661 patients who met the inclusion criteria for diagnosis of PsA, the mean age was 55.8 years and 60.2% were women. Compared with controls, patients with PsA had an increased history of coding for arthritis and skin issues including osteoarthritis (OA; 48% vs 22%), rheumatoid arthritis (RA; 18% vs 2%), inflammatory polyarthropathy (IA; 18% vs 1%), and psoriasis (60% vs 2%) (Figure 1A). PsA patients without a prior diagnosis of psoriasis had higher levels of coding for other forms of arthritis compared to PsA patients with psoriasis including OA (53% vs 45%), RA (27% vs 13%), and IA (26% vs 12%) (Figure 1B). For many patients, diagnoses of different types of arthritis, axial symptoms, and tendonitis/enthesitis steadily increased over time prior to their PsA diagnosis (Figure 2A). In particular, there was a sharp rise in psoriasis diagnoses preceding the diagnosis of PsA and smaller increases in diagnoses of OA and IA prior to PsA diagnosis. Rheumatology visits were much more common just before the diagnosis of PsA (Figure 2B). Diagnoses made prior to diagnosis of PsA differed by the type of provider patients seen. Dermatologists were less likely than other providers to enter codes for arthritis and musculoskeletal issues, while rheumatologists were unlikely to code for psoriasis but had a fairly even distribution across different types of arthritis. General practitioners focused more on axial symptoms and general musculoskeletal codes than arthritis diagnoses (Figure 3A). PsA was most commonly diagnosed by rheumatologists (40%) but was diagnosed in 22% and 7% of cases by general practitioners and dermatologists, respectively (Figure 3B).
Conclusion: Rheumatologists, general practitioners, and dermatologists were responsible for diagnosing two-thirds of patients with PsA. Musculoskeletal symptoms and potential misdiagnoses are common in the years preceding diagnosis of PsA and the diagnoses and codes entered prior to PsA diagnosis varied by provider type.
To cite this abstract in AMA style:
Ogdie A, Rozycki M, Arndt T, Shi C, Kim N, Hur P. Longitudinal Analysis of the Patient Pathways to Diagnosis of Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/longitudinal-analysis-of-the-patient-pathways-to-diagnosis-of-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-analysis-of-the-patient-pathways-to-diagnosis-of-psoriatic-arthritis/