Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Seronegative rheumatoid arthritis (RA) is a heterogenous disease distinct from seropositive RA regarding genetic risk factors, pathobiology, and prognosis. Notably, recent studies have shown an increasing incidence of seronegative RA. However, there is limited data regarding long-term outcomes. The purpose of this study was to determine the cumulative incidence of diagnosis switching, drug-free remission (DFR), and initiation of a biologic or targeted synthetic disease modifying anti-rheumatic drug (b/tsDMARD) in patients with seronegative RA.
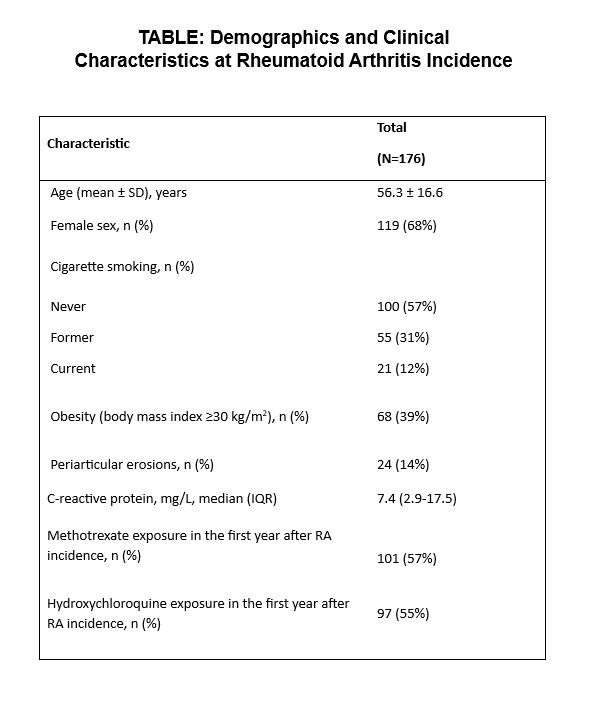
Methods: This study evaluated the 10-year cumulative incidence of various prognostic features in patients with seronegative RA using a population-based inception cohort. All adult patients with incident seronegative (rheumatoid factor-/anti-cyclic citrullinated peptide antibody-) RA between January 1, 2005, through December 31, 2014, meeting the 1987 and/or the 2010 American College of Rheumatology classification criteria were included. Data was collected through manual chart review. A change in diagnosis was defined as a persistent change in diagnosis by a rheumatologist. As clinical disease activity indices were not available for all patients, DFR was defined as a period of least 6 months where the patient was no longer on treatment for RA and did not have evidence of active inflammatory arthritis on evaluation by a rheumatologist. Aalen-Johansen methods were used to calculate the 10-year cumulative incidence of a change in diagnosis, adjusting for the competing risk of death, and of DFR and initiation of a b/tsDMARD, adjusting for the competing risks of death or change in diagnosis.
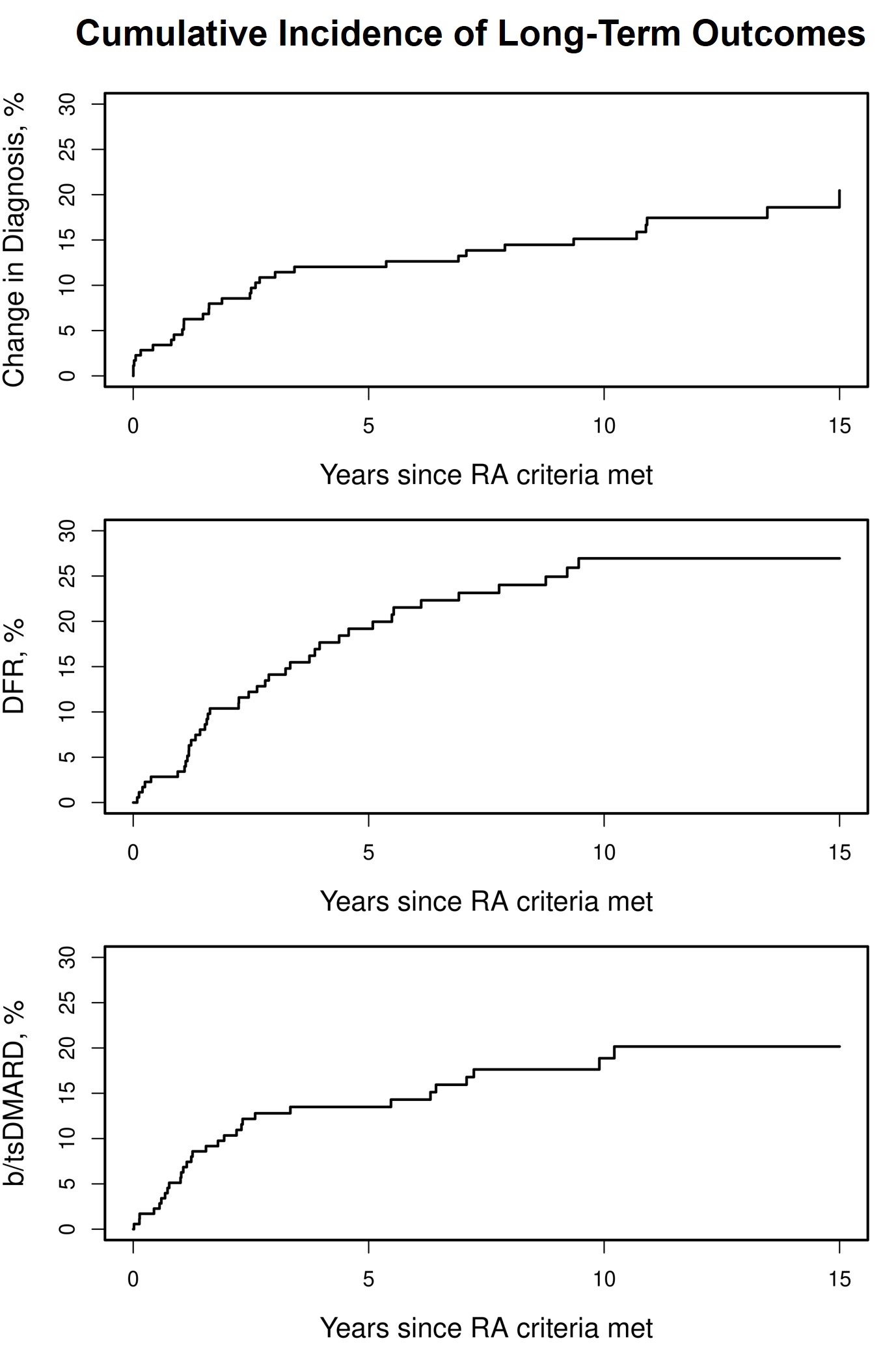
Results: A total of 176 patients (68% female) were included (Table). During a median of 11.8 years of follow-up, 32 patients had a change in diagnosis, 40 reached DFR, and 30 initiated a b/tsDMARD. The 10-year cumulative incidence of a change in diagnosis was 15.1% (95% confidence interval [CI]: 10.6-21.6%; Figure). New diagnoses included (number of patients) spondyloarthropathy (11), seropositive RA (6), osteoarthritis (5), crystalline arthritis (3), connective tissue disease (3), infection related arthropathy (1), paraneoplastic arthropathy (1), remitting seronegative symmetrical synovitis with pitting edema (1), and sarcoidosis (1). The 10-year cumulative incidence of DFR and initiation of a b/tsDMARD was 26.9% (95% CI: 20.5-35.4%) and 18.9% (95% CI: 13.4-26.5%), respectively (Figure). Among 90 patients with incident RA between 2010-2014, there was no significant difference in the cumulative incidence of a change in diagnosis or DFR between patients who met the 2010 classification criteria (n=57) versus those who only met the 1987 criteria (n=33).
Conclusion: After an initial diagnosis of seronegative RA, only a small portion of patients had a change in diagnosis by year 10. The most common change in diagnosis was to a spondyloarthropathy, followed by seroconversion to seropositive RA. About a quarter of patients will experience DFR.
To cite this abstract in AMA style:
Kimbrough B, Crowson C, Achenbach S, Myasoedova E. Long-Term Outcomes in Seronegative Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/long-term-outcomes-in-seronegative-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-outcomes-in-seronegative-rheumatoid-arthritis/