Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Patients with rheumatoid arthritis (RA) have an increased risk of atherosclerotic cardiovascular disease (ASCVD) compared to the general population and RA is considered a risk-enhancing factor in ASCVD. Other risk factors like dyslipidemia, hypertension, smoking, diabetes, and obesity put RA patients at additional increased risk of ASCVD and must be assessed frequently. 2018 American Heart Association/American College of Cardiology (AHA/ACC) guidelines recommend that in adults 40-75 years of age without diabetes mellitus and with LDL-C levels ≥70 mg/ dL, at a 10-year ASCVD risk of ≥7.5%, start a moderate-intensity statin if a discussion of treatment options favors statin therapy. Risk-enhancing factors, like RA, favor initiation of statin therapy. The goal of our study was to quantify the rate of lipid screening and statin use in RA patients and to calculate ASCVD risk scores to determine who would benefit from statin initiation. With this baseline information we plan to create a QI intervention to improve screening and statin use in our patient population.
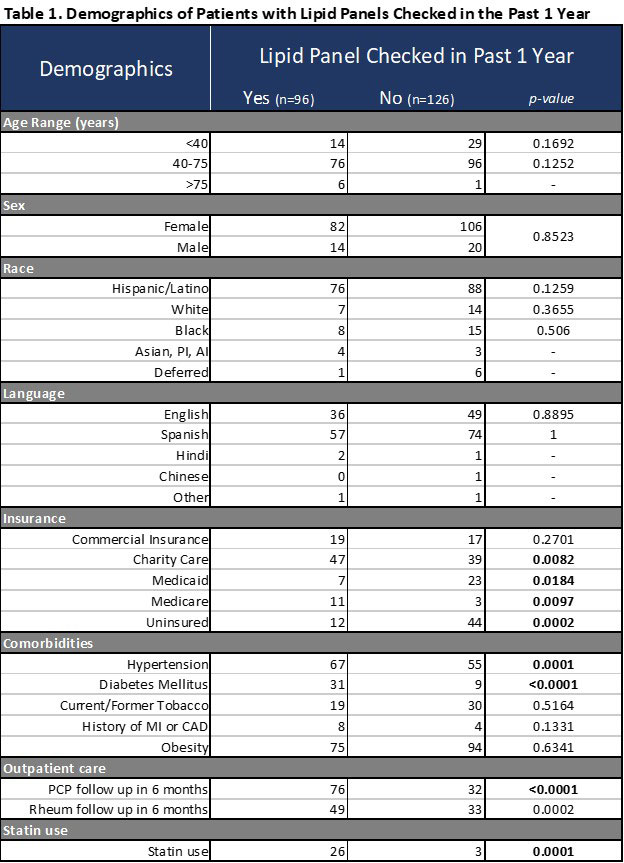
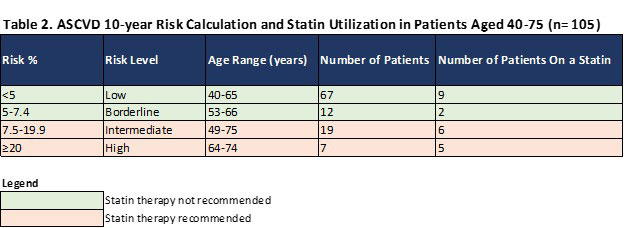
Methods: We performed a retrospective chart review on RA patients seen in our clinic from September 2018 – November 2020. Our clinic is located in a federally qualified health center and patients with RA meet the 2020 American College of Rheumatology (ACR) Classification Criteria. We collected demographic data, modifiable CV risk factors, follow-up information, statin use and annual lipid panel screening. Fisher’s Exact Test was used to compare demographics for patients who have had a lipid panel checked in the past year and those who have not. For patients ages 40-75 with documented lipid panels, ASCVD 10-year risk scores were calculated using the 2013 ACC/AHA cardiovascular risk calculator based on the Pooled Cohort Equation. Results of risk scores were organized as low, borderline, intermediate, or high risk as per ACC cut-offs. For patients who did not have lipid panels within the past year, ASCVD risk scores were calculated from the most recent lipid panel in the system if available.
Results: Two hundred twenty-two patients with RA were seen in rheumatology clinic and 43% had a lipid panel checked in the last year. Table 1 shows patients who had a lipid panel checked within 1 year had a significantly higher rate of hypertension and diabetes. Patients without a lipid panel in the last year were more likely to be uninsured and not have seen a primary care provider (PCP) in the past 6 months. Out of 26 patients who should be on a statin based on AHA/ACC guidelines, only 42.3% are on a statin (Table 2).
Conclusion: Our data has identified a population of RA patients at higher risk for CV disease who should be on a statin. Our next step is to develop a QI intervention to increase risk factor and lipid panel screening, and to initiate statin therapy based on risk scores in this high risk population.
To cite this abstract in AMA style:
O'Neill C, Patel V. Lipid Screening and Statin Use in Rheumatoid Arthritis Patients in an Underserved Population [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/lipid-screening-and-statin-use-in-rheumatoid-arthritis-patients-in-an-underserved-population/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lipid-screening-and-statin-use-in-rheumatoid-arthritis-patients-in-an-underserved-population/