Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: JIA is the most common rheumatic disease of childhood, but recent data on diagnostic trends in the US are lacking. Furthermore, the impact of the ICD-9/ICD-10 transition on the rates of JIA diagnoses is unclear. We sought to characterize recent trends in JIA claims, including changes related to the US International ICD-9/ICD-10 transition in late 2015.
Methods: We studied JIA diagnoses within administrative claims data on commercially insured children under age 18 from 14 geographically diverse US states in the HealthCore Integrated Research Database (2006-2019). JIA diagnoses were defined by claims with diagnostic codes (ICD-9 696.0, 714, or 720; ICD-10 L40.5, M05, M06, M08, or M45), requiring at least 1 inpatient claim or 2 outpatient claims between 8 and 52 weeks apart. Incident diagnoses were defined as having at least 6 months of baseline data without previous JIA claim; prevalent diagnoses could have occurred at any time. Incidence and prevalence of JIA were calculated quarterly 2006-2019, excluding 6 months before and 6 months after the ICD-9/10 transition to limit transitional coding errors. Trends and changes in level around the ICD-9/10 transition were analyzed by single-group interrupted time-series using ordinary least-squares segmented regression.
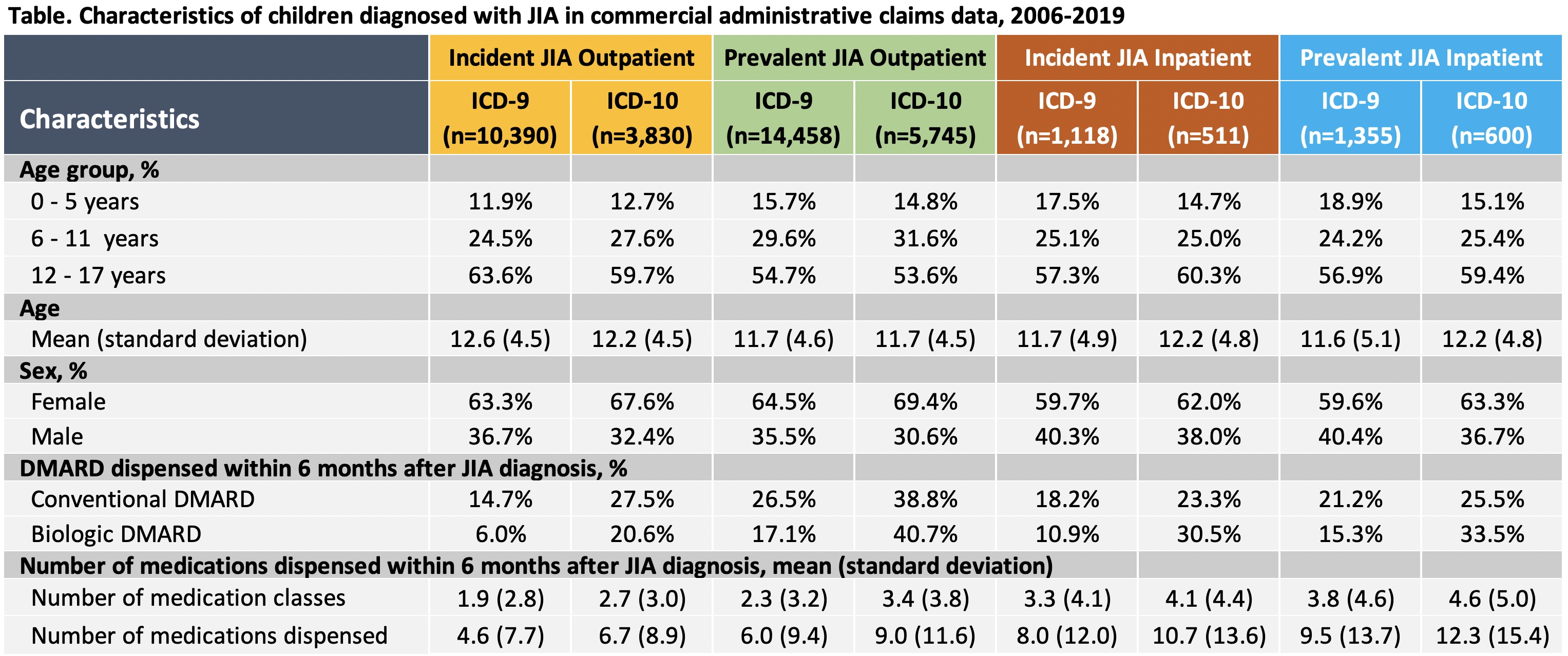
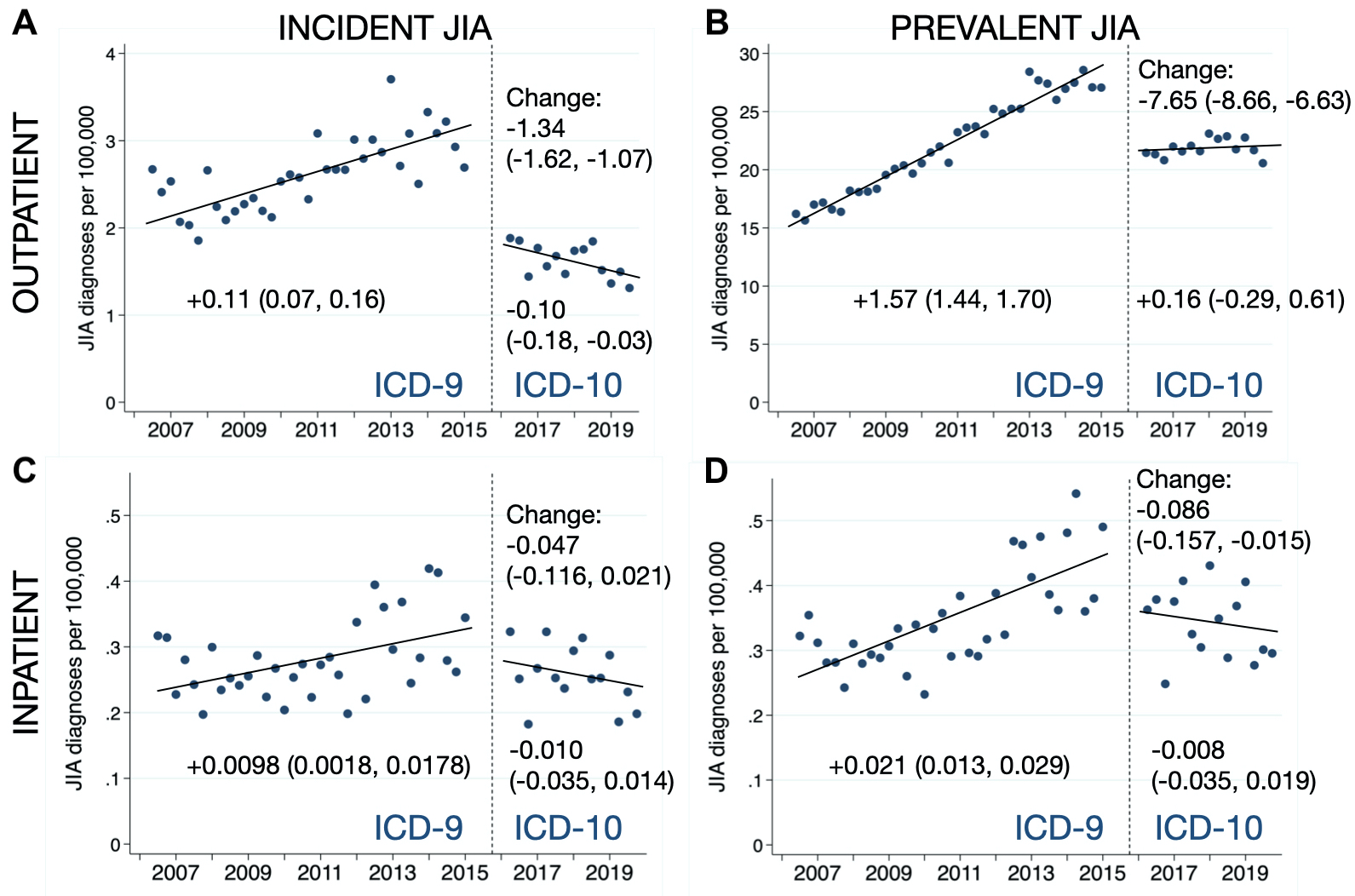
Results: Of 26.5 million children identified, 22,158 had claims for JIA by ICD-9 or ICD-10 code in any setting (0.084%). Over half of children diagnosed with JIA were 12-17 years old, and approximately 2/3 were female (Table). ICD-9-based incident and prevalent diagnoses of JIA steadily increased in both outpatient and inpatient settings (Figure). Rates of JIA, both incident and prevalent, dropped abruptly in both outpatient and inpatient settings at the time of the ICD-9/10 transition (Figure). In outpatient settings, ICD-10-based incident JIA diagnoses have declined since then, whereas prevalent JIA diagnoses have remained stable (Figure). There have been modest, but not statistically significant, declines in ICD-10-based diagnoses from inpatient settings (Figure). Rates of recorded conventional and biologic DMARD use were higher among children diagnosed by ICD-10 code than children diagnosed by ICD-9 code (Table).
Conclusion: Among commercially insured children, apparent incident and prevalent rates of claims for JIA declined abruptly with the US transition from ICD-9 to ICD-10, likely reflecting an artifact of changes in the sensitivity and specificity of coding practices. The higher prevalence of DMARD use by children diagnosed with JIA in the ICD-10 era could suggest greater diagnostic specificity, but the uncertain validity of both ICD-9 and ICD-10 claims warrants further research. New JIA diagnoses appeared to rise until 2015 and fall since 2016; more work is needed to establish to what extent these trends reflect temporal changes in coding practices versus true changes in JIA epidemiology.
 JIA diagnosis trends ACR abstract.001.jpeg”
JIA diagnosis trends ACR abstract.001.jpeg”
To cite this abstract in AMA style:
Horton D, Parlett L, Huang C, Crystal S, Davidow A, Gerhard T, Rose C, Haynes K, Strom B. JIA Diagnoses and Trends from 2006-2019: Has the U.S. ICD-9-to-ICD-10 Transition Created Coding Artifacts? [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/jia-diagnoses-and-trends-from-2006-2019-has-the-u-s-icd-9-to-icd-10-transition-created-coding-artifacts/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/jia-diagnoses-and-trends-from-2006-2019-has-the-u-s-icd-9-to-icd-10-transition-created-coding-artifacts/