Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Gout is a chronic inflammatory arthritis induced by hyperuricemia and manifested by recurrent acute flares of debilitating joint pain when left untreated. Allopurinol is often used as long-term urate lowering therapy. Improper discontinuation of allopurinol leads to worsening flares, disability, poor quality of life, and frequent use of acute care facilities. (1, 2) We performed a qualitative analysis of rates of discontinuation of allopurinol during hospitalizations at an academic hospital to develop a continuous improvement model.
Methods: We leveraged electronic health records for data on gout patients admitted to the university hospital from 2019-2024. Patients who were on allopurinol as a home medication but were taken off during hospitalization and not renewed after discharge, were included to calculate the rates of discontinuation. Lean thinking methodology with A3 process mapping for root cause analysis (RCA) was utilized. First, we identified stakeholders involved in medication reconciliation and invited them to participate in an anonymous survey with reasons for discontinuation. Admission diagnoses and patient comorbidities were included as potential reasons for discontinuation. Next, we crafted countermeasures as actionable recommendations to be implemented at an institutional level. We analyzed data from 2019-2024 in patients with allopurinol on admission to understand if educational countermeasures influenced discontinuation rates in the subsequent years. Groups were separated into 2019-2020 (pre-intervention) and 2021-2024 (post-intervention).
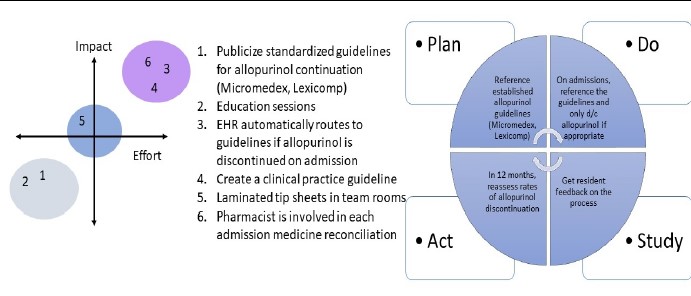
Results: A total of 2138 patients were hospitalized, and of these 364 (17%) did not receive allopurinol during their admission. Based on the survey data, clinicians chose to discontinue allopurinol due to the following factors – acute gout flare, renal impairment, gastrointestinal issues, cytopenia, drug interactions, NPO status, and always discontinued the medication. The RCA revealed layers of reasoning at various levels of the medication reconciliation process which impacted the decision-making algorithm. Several actionable and high-impact recommendations emerged as countermeasures (Figure 1). Laminated tipsheets on gout-related therapies were posted in all inpatient team rooms as an educational guide and management guidelines were reinforced with pharmacy teams. We found a continued trend toward non-renewal of Allopurinol prescriptions in the post intervention period upon discharge (p >0.05).
Conclusion: There is ongoing evidence of suboptimal management with frequent discontinuation of allopurinol during hospitalizations (2019-2024) at an academic university setting. This leads to higher rates of post-discharge gout flares requiring unnecessary resource utilization. Educational sessions were well received, however, high-impact interventions that utilize a ‘forced function’ approach as a continuous improvement strategy, are likely to significantly impact patient outcomes at an institutional level.
To cite this abstract in AMA style:
Tancer S, Al Dulaijan B, Khanna P. Inpatient Discontinuation of Allopurinol – A Quality Improvement (QI) Initiative [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/inpatient-discontinuation-of-allopurinol-a-quality-improvement-qi-initiative/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inpatient-discontinuation-of-allopurinol-a-quality-improvement-qi-initiative/