Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with systemic lupus erythematosus (SLE) have increased mortality compared to the general population. As outcomes related to disease control have improved, this mortality difference has been explained increasingly by higher rates of cardiovascular and renal disease. Blood pressure visit-to-visit variability (BPV) has emerged as a risk factor for cardiovascular and renal outcomes in the general population but little is known about this relationship in SLE. We hypothesized that SLE patients have greater BPV than control subjects and that BPV is associated with higher comorbidity burden and increased mortality in SLE.
Methods: We identified a cohort of patients with SLE using a previously validated algorithm (PPV 94%) from a de-identified version of an academic medical center’s electronic health record (EHR) and then frequency-matched (age, race, and sex) SLE patients to a control group in a ~5:1 control-case ratio. We excluded patients with fewer than three visits or age <18 years at the time of the first relevant ICD9 code (710.0 for SLE, any code for controls). We extracted demographic variables (age, race, and sex), ICD9 codes, laboratory results, and outpatient blood pressure values from the EHR. We compared BPV in SLE patients and controls. The primary outcome was systolic blood pressure coefficient of variation. Secondary outcomes included standard deviation, average real variation, and successive variation for both systolic and diastolic blood pressure. Second, we examined the association between BPV with clinical characteristics and mortality in patients with SLE.
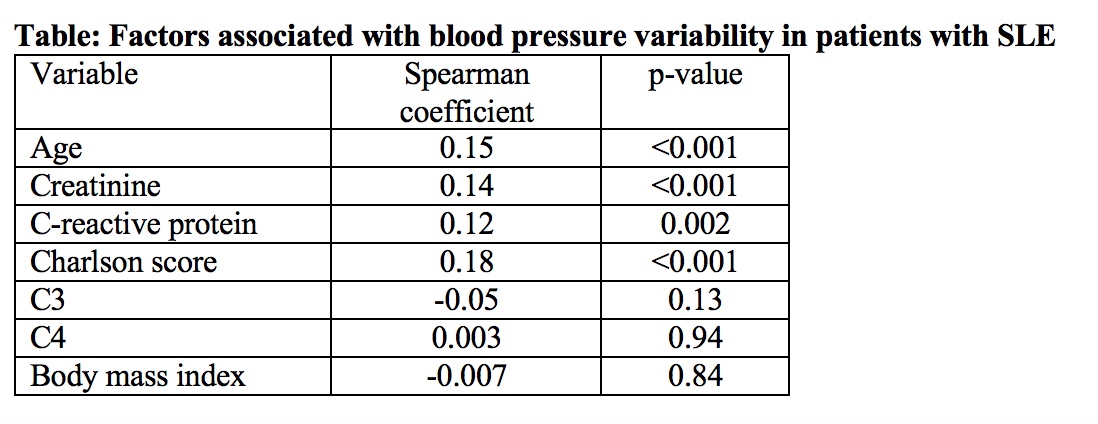
Results: 899 patients with SLE and 4172 controls met inclusion criteria. Age, sex, and race were similar among the SLE and control groups. Patients with SLE had higher systolic BPV 9.7% [7.8-11.8] than the control group 9.2% [7.4-11.2], p<0.001 measured by coefficient of variation. All other measures of BPV were significantly higher in patients with SLE than in controls. In SLE patients, BPV correlated significantly with age, creatinine, C-reactive protein, and the Charlson comorbidity score; but not with C3, C4, and body mass index (Table). There was no statistically significant difference in BPV by sex, but Caucasian SLE patients [9.6% (7.9-11.4)] had lower BPV than SLE patients who were African-American [10.3% (7.9-12.9)] or patients from other races [10.4% (7.6-12.3)], p=0.015. Over a median follow-up of 6.5 years, 91 patients died. After adjustment for age, sex, race, and baseline Charlson comorbidity score, higher BPV was associated with death in patients with SLE [OR=1.24, 95% CI 1.16-1.33, p<0.001].
Conclusion: SLE patients had a higher BPV than the control group. In patients with SLE, higher BPV was associated with older age, higher creatinine, inflammation, comorbidity index, and mortality.
To cite this abstract in AMA style:
Reese T, Dickson A, Neal JE, Gandelman JS, Khan OA, Barnado A, Dupont W, Stein CM, Chung CP. Increased Blood Pressure Visit-to-Visit Variability in Patients with Systemic Lupus Erythematosus: Association with Inflammation, Comorbidities and Increased Mortality [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/increased-blood-pressure-visit-to-visit-variability-in-patients-with-systemic-lupus-erythematosus-association-with-inflammation-comorbidities-and-increased-mortality/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-blood-pressure-visit-to-visit-variability-in-patients-with-systemic-lupus-erythematosus-association-with-inflammation-comorbidities-and-increased-mortality/