Session Information
Date: Friday, March 31, 2023
Title: Poster Breakout 4 - JDM & Scleroderma: Clinical & Therapeutic Aspects
Session Type: Breakout Session
Session Time: 4:30PM-5:00PM
Background/Purpose: There is a paucity of data on pediatric rheumatic disease (PRD) in low and middle-income countries (LMIC), creating a false perception of low prevalence when this gap is driven by limited diagnostic capacities, scarcity of pediatric rheumatologists, and limited awareness of PRD. Juvenile dermatomyositis (JDM) can cause significant morbidity and irreversible damage when inadequately treated, resulting in medical, social, and economic burden on patients, families, and healthcare systems, particularly in LMIC. The few studies of JDM in Africa suggest high rates of severe manifestations, including calcinosis and pulmonary involvement. The objective of this survey is to better understand the scope of JDM burden in Africa by obtaining an overview of JDM and comparing this to data in previously published work.
Methods: A survey was distributed to members of the African League of Associations for Rheumatology (AFLAR; n=233) and Paediatric Society of the African League Against Rheumatism (PAFLAR; n=130) via WhatsApp groups. Respondents were queried about the total number of JDM patients seen currently or within the last 10 years; morbidities and clinical outcomes, including calcinosis, interstitial lung disease (ILD), clinically inactive disease, remission, and death; and availability and accessibility of diagnostic tools and medications.
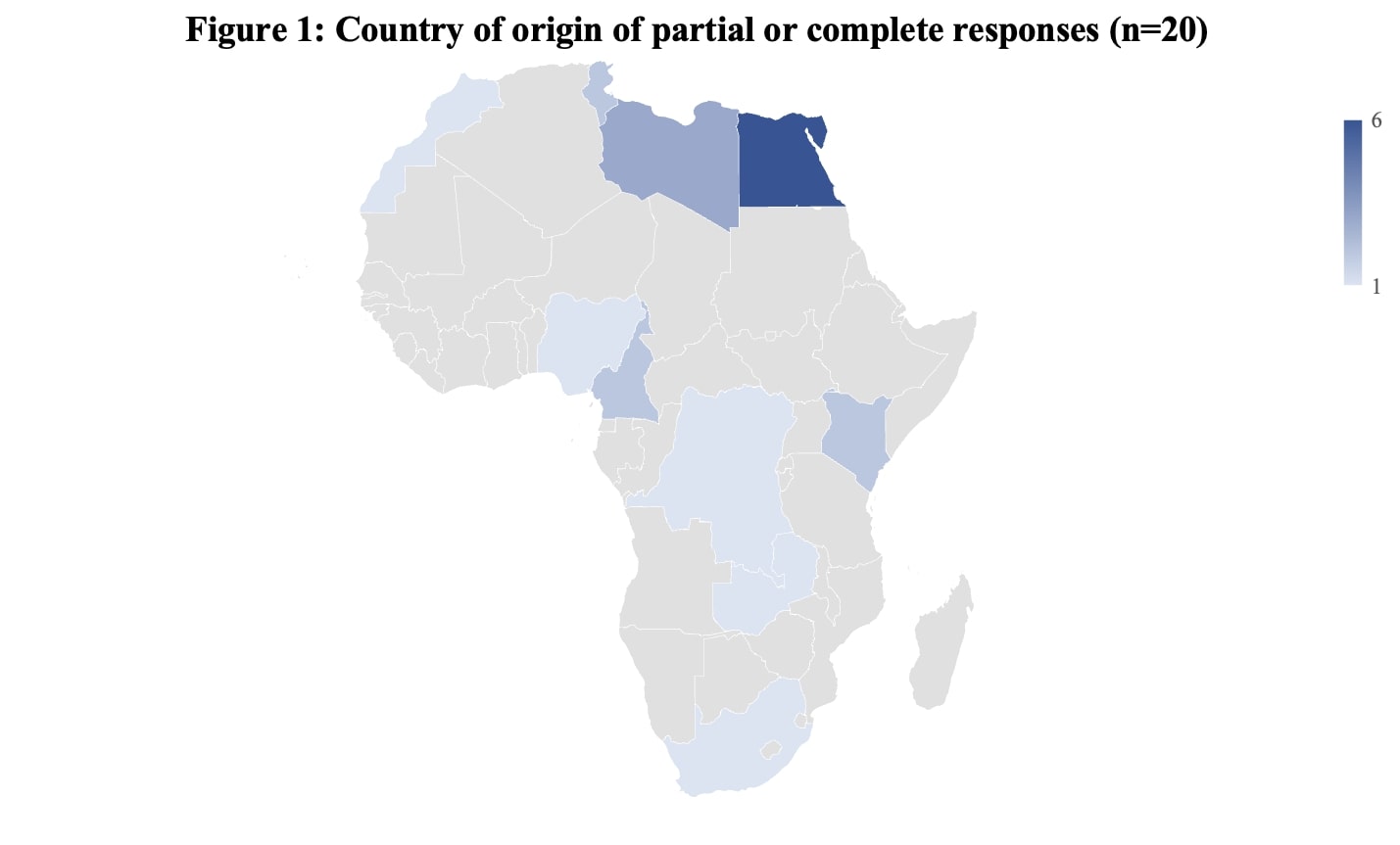
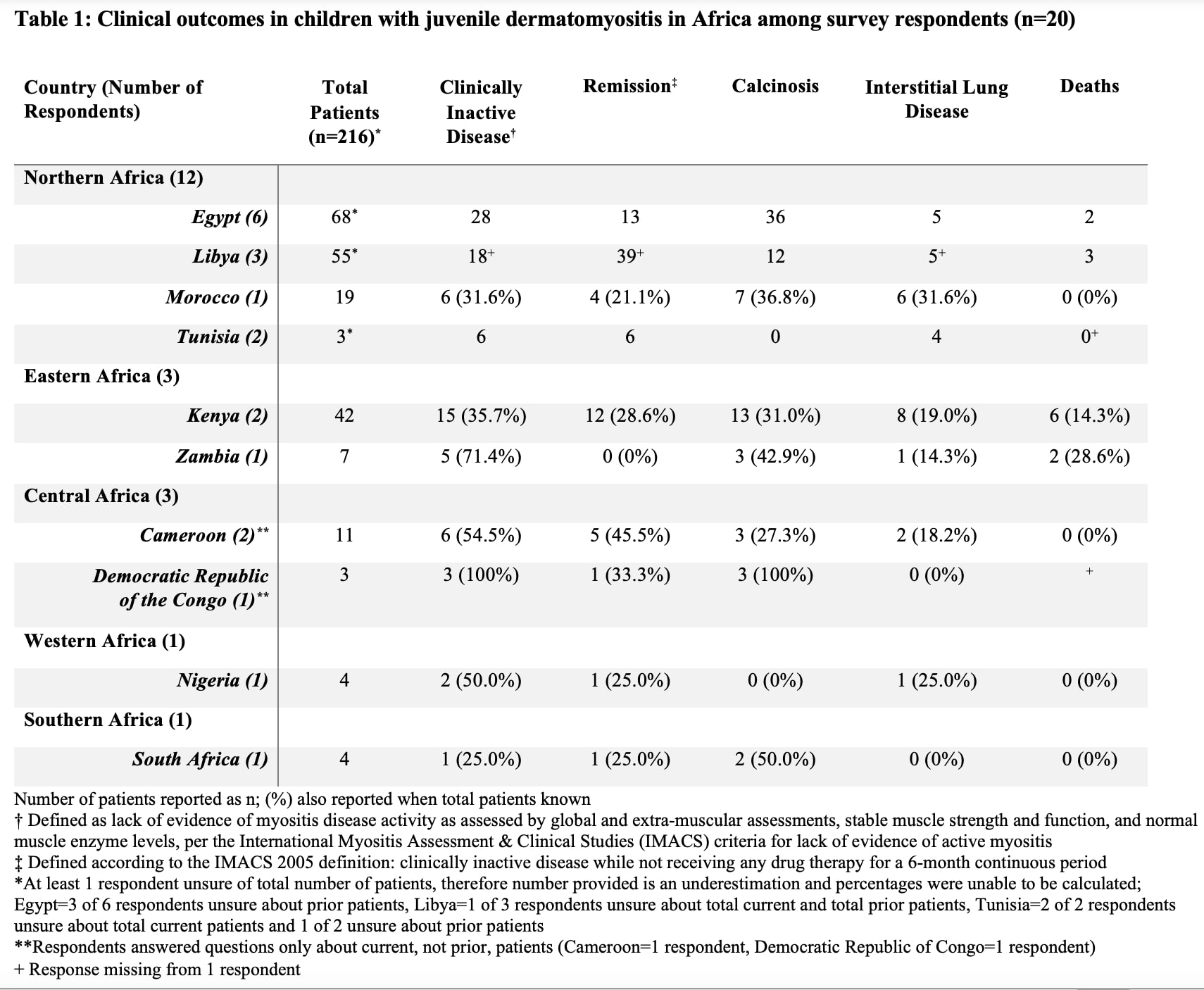
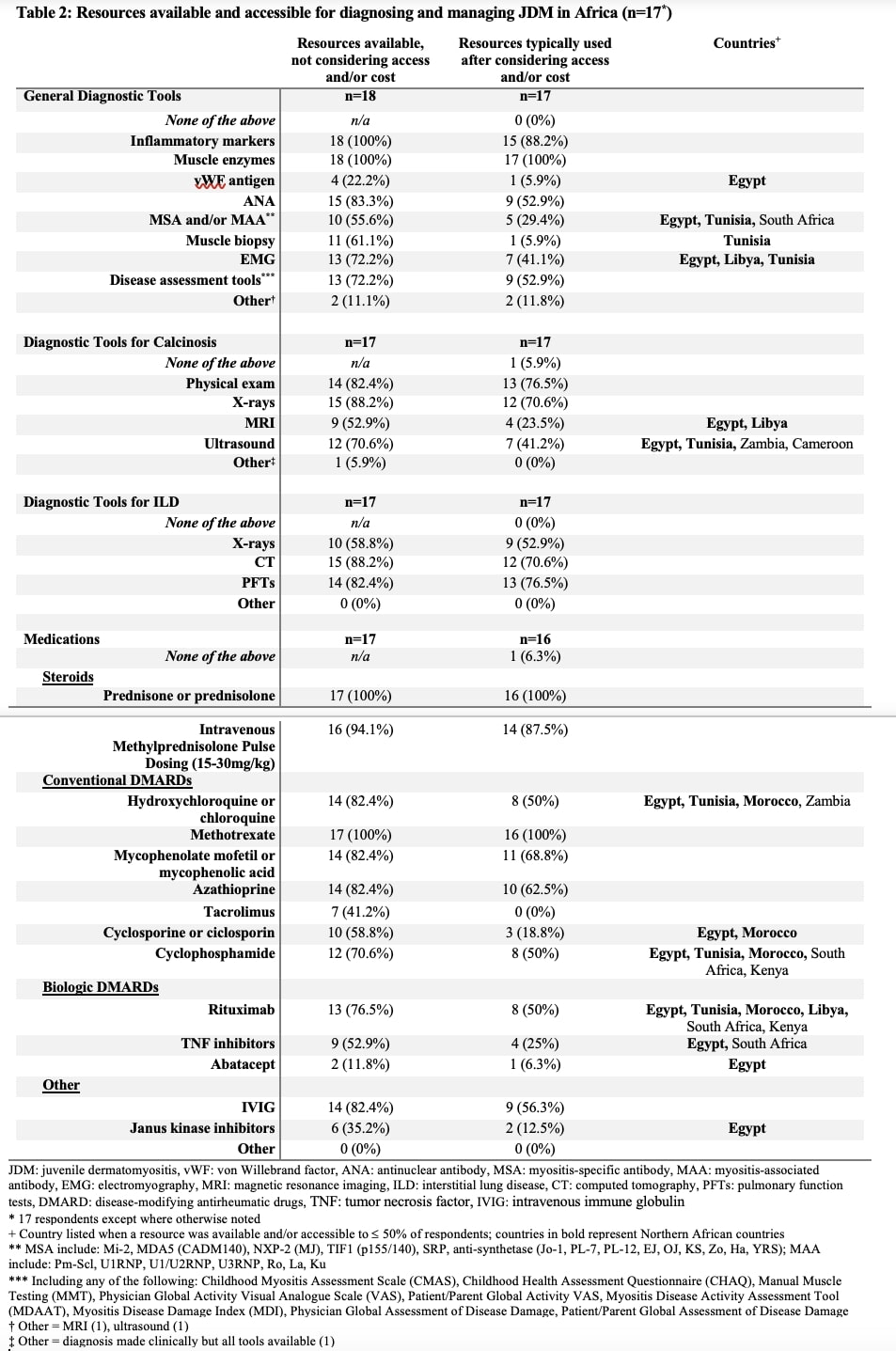
Results: A total of 43 (12%) individuals started the survey, with 4 (9%) partially and 16 (37%) fully completing it, describing 216 JDM patients. One general pediatrician participated; the remainder were adult (n=10; 50%), pediatric (n=7; 35%), or adult/pediatric (n=2; 10%) rheumatologists. Respondents represented the 5 regions of Africa, primarily Northern Africa (n=12; 60%) (Figure 1). Mortality was reported at 14% and 29% in Kenya and Zambia, respectively (Table 1). Many respondents identified limited availability of medications (56%), unfamiliarity with JDM by caregivers (69%) and other medical providers (44%), and delayed presentation to care (75%). Access and/or cost limited use of diagnostic tools and medications (Table 2). 13 diagnostic tools and medications were typically used by 50% or fewer of respondents, the majority (69%) of which are accessible in only Northern or Southern African countries. Despite the lack of cost or other apparent access barriers, disease assessment tools are used by only 53% of respondents.
Conclusion: This is the first study to explore JDM on a broad scale across the African continent. We identified 216 African children with JDM within the past 10 years, exceeding the previously published reports of 196 JDM patients seen in the last 25 years and likely still underestimating prevalence. Our results suggest substantially higher rates of severe disease, with mortality rates in some countries vastly different from the 1-3% reported in high-income countries. Many respondents were limited in their capacity to diagnose and treat JDM, but there was a wide range across African regions. This survey highlighted important possible differences in disease manifestations and outcomes that warrant further study. Future collaboration with our African colleagues is critical to raise awareness of JDM to ultimately improve disease severity and outcomes.
To cite this abstract in AMA style:
Perfetto J, Lewandowski L, Wahezi D, Scott C, Migowa A. Identifying and Understanding JDM in Africa: A Survey of Rheumatology Care Providers from Africa [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/identifying-and-understanding-jdm-in-africa-a-survey-of-rheumatology-care-providers-from-africa/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-and-understanding-jdm-in-africa-a-survey-of-rheumatology-care-providers-from-africa/