Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Cardiac involvement in systemic sclerosis (SSc) is one of the leading causes of scleroderma-associated death. There are limited data examining risk factors for incident cardiomyopathy or for cardiac recovery in patients with SSc.
Methods: Patients in a large North American longitudinal scleroderma cohort with at least two echocardiograms were included. We identified predictor variables associated with incident cardiomyopathy (ejection fraction (EF) ≥ 50% declining to < 50%) and severe cardiomyopathy (EF > 35% dropping to ≤ 35%) by fitting two multivariate logistic regression models. Time-varying and invariant variables were used to model EF transitioning from one state to another. For time-varying variables, values captured most recently prior to each EF transition were used. Variables that associate with cardiac recovery (EF < 50% to ≥ 50%, EF ≤ 35% to > 35%) were identified by fitting multivariate logistic regression models using important variables identified from random forest models. We reviewed the medical records of the 139 patients whose EF ≤ 35% was ever to further characterize the etiology of severe cardiomyopathy.
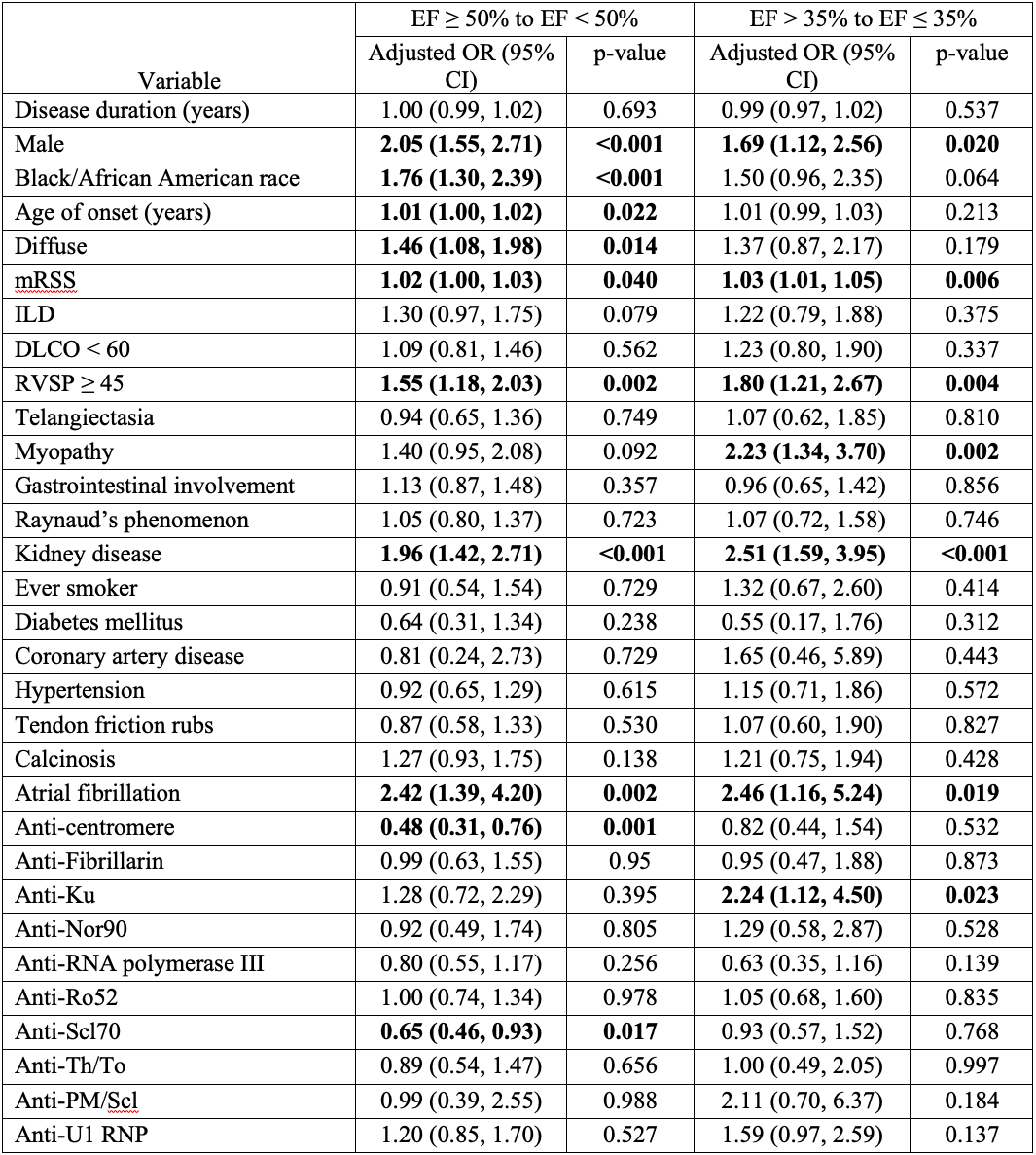
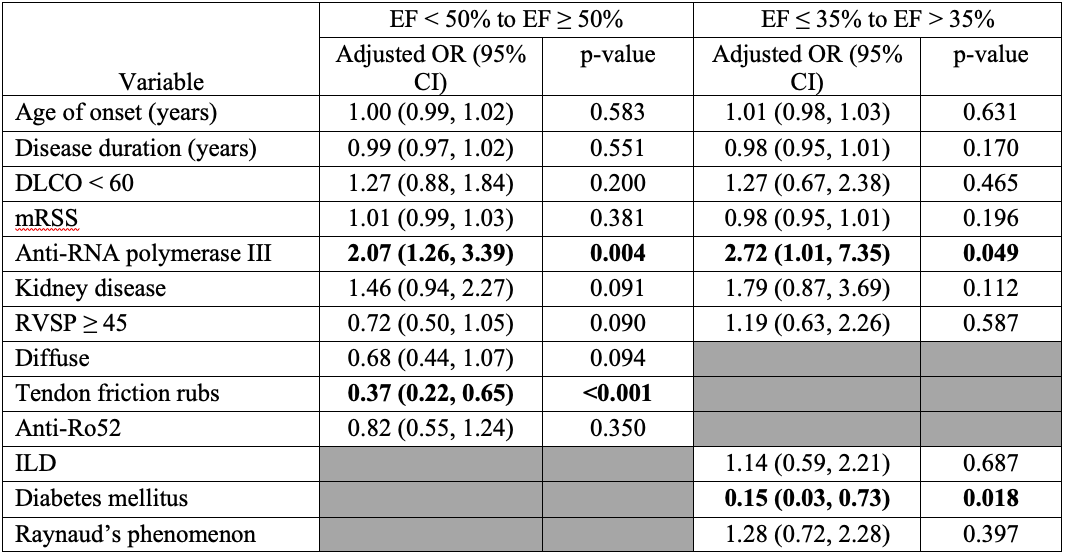
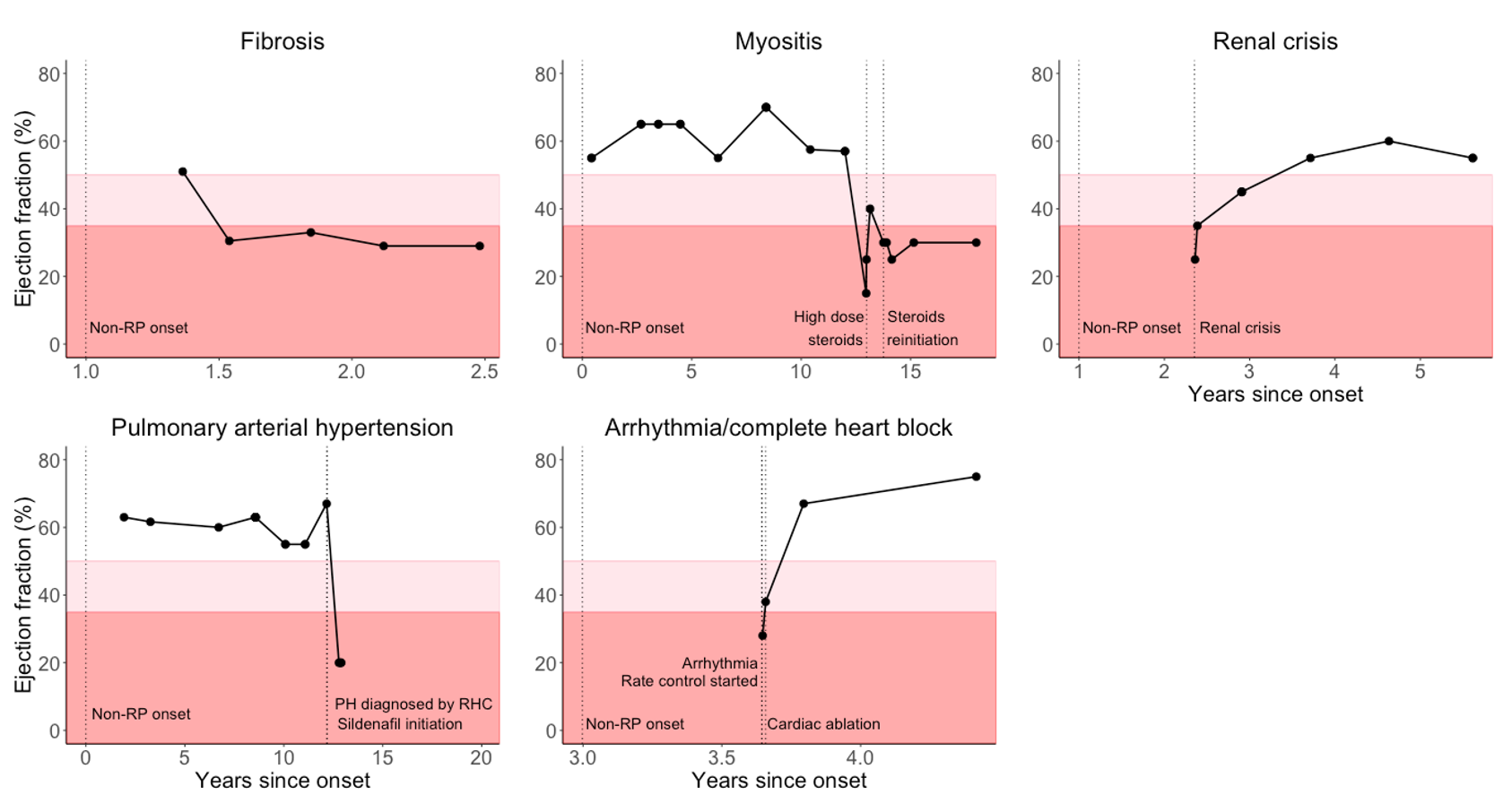
Results: 2,303 patients in the cohort with at least two echocardiograms were included, and 13,209 echocardiograms were analyzed. Male sex, Black race, diffuse skin involvement, onset age, higher mRSS, RVSP ≥ 45, kidney disease, and atrial fibrillation were associated with increased odds of incident cardiomyopathy (EF < 50%), while anti-centromere and anti-Scl70 were protective (Table 1). Male sex, anti-Ku, higher mRSS, RVSP ≥ 45, skeletal myopathy, kidney disease, and atrial fibrillation were associated with higher odds of incident severe cardiomyopathy (EF ≤ 35%). When previous EF was below 50%, tendon friction rubs were associated with lower odds of cardiac recovery, and anti-RNA polymerase III (POLR3) with higher odds of cardiac recovery (Table 2). When previous EF was less than or equal to 35%, diabetes was associated with lower odds of recovering to EF > 35%, and anti-POLR3 with higher odds. The most common causes of EF ≤ 35% identified through medical record review were ischemic heart disease, conduction/arrhythmia-related, myocarditis, fibrosis, right heart failure from pulmonary hypertension, infection, and renal crisis. Representative trajectories of patients with scleroderma-related cardiomyopathy are shown in Figure 1.
Conclusion: This study provides the most detailed analysis of factors associated with varying degrees of incident cardiomyopathy in SSc using time-varying predictor variables and is the only study to explore factors associated with left ventricular recovery. Distinct demographic, scleroderma-specific and cardiac risk factors associate with increased risk of incident cardiomyopathy in scleroderma. Anti-POLR3 antibodies were associated with EF recovery.
To cite this abstract in AMA style:
Kim J, Wallwork R, Richardson C, Woods A, Mukherjee M, Hsu S, Paik J, Mecoli C, Hummers L, Wigley F, Zeger S, Shah A. Identification of Risk Factors for Incident Cardiomyopathy in Patients with Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/identification-of-risk-factors-for-incident-cardiomyopathy-in-patients-with-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-risk-factors-for-incident-cardiomyopathy-in-patients-with-systemic-sclerosis/