Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Medication non-adherence is associated with worse autoimmune disease outcomes; however, it is unknown whether adherence rates related to cost barriers differ across diseases and subpopulations. This is part of an ongoing study evaluating the effects of cost-related medication non-adherence (CRMNA) in immunosuppressed patients. In prior analyses, we found that patients with medical immunosuppression and chronic disease were more likely to report CRMNA compared to the group without medical immunosuppression. The purpose of this study is to estimate predicted probabilities of CRMNA across age groups, and to evaluate how people in poor health, identified as a high risk population in our study, experience CRMNA.
Methods: We performed a cross-sectional study using the 2022 National Health Interview Study (NHIS). Survey respondents were categorized into three groups: medically immunosuppressed without other chronic health conditions, the presence of other chronic health conditions and not medically immunosuppressed, and both medically immunosuppressed and containing other chronic health conditions. Multivariable logistic regression was used to evaluate the association of immunosuppression use with CRMNA, accounting for survey weighting and complex survey design and predicted probabilities of CRMNA were estimated for age groups. Subgroup analyses were performed among people receiving immunosuppression who described poor health.
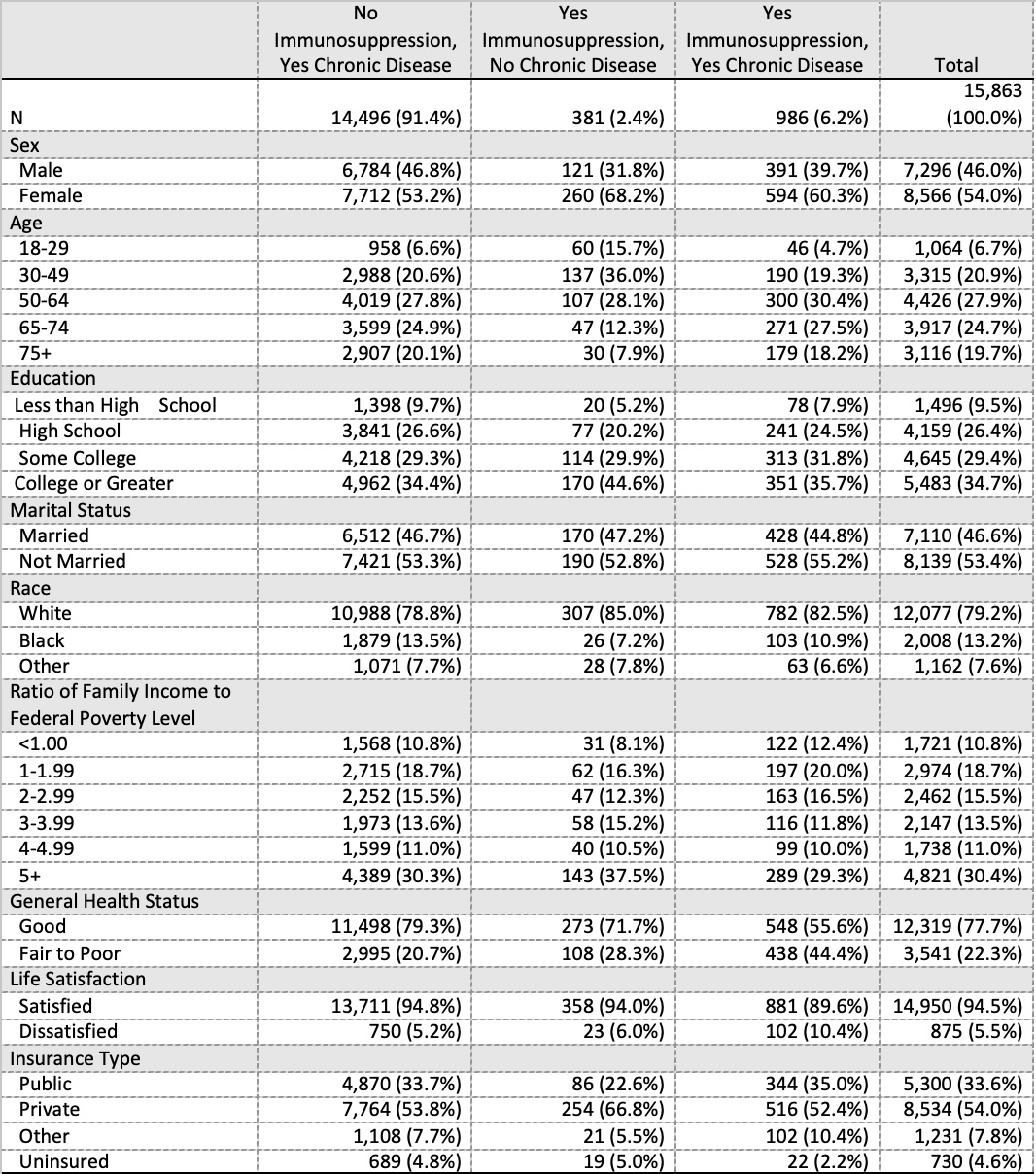
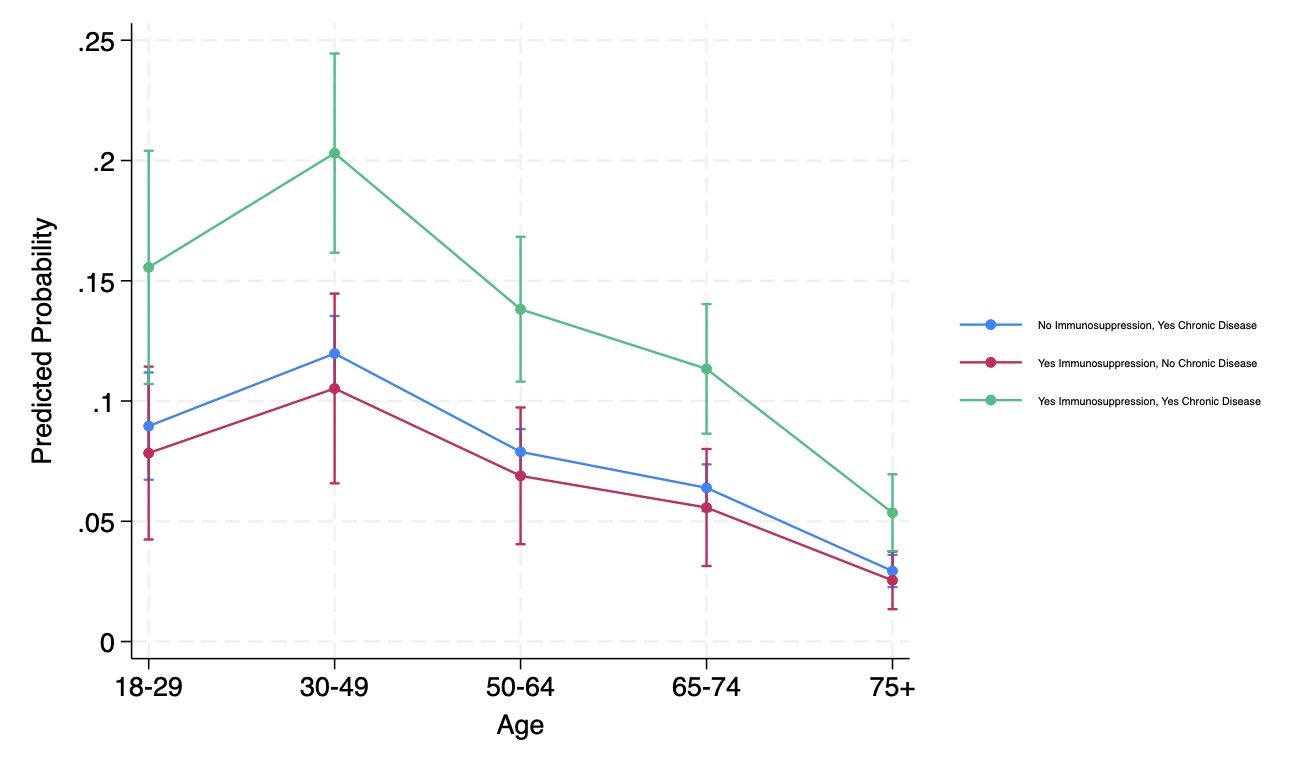
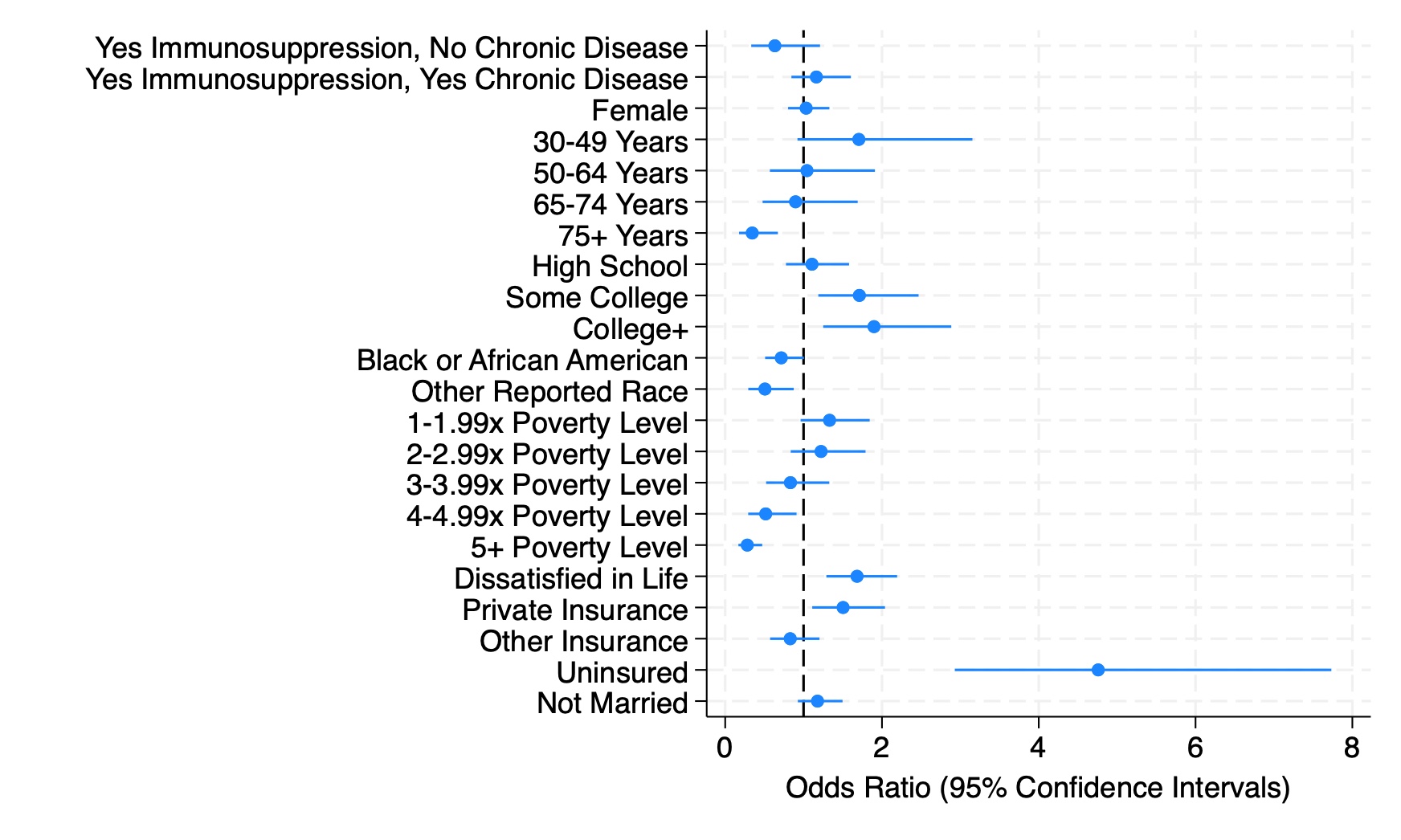
Results: In our unweighted sample of 15,863 adults, 54% were female, 13.2% self-identified as Black, 33.6% were publicly insured and 10.8% were below the federal poverty level (Table 1). In the weighted, multivariate model accounting for all covariates, the group with medical immunosuppression and chronic disease reported a higher odds ratio for the development of CRMNA (OR 1.5, 95% CI [1.17, 1.91], p< 0.01). The probability of reporting CRMNA was significantly higher in the group with immunosuppression and chronic disease, especially in younger age groups (Figure 1). The predicted probability of a 30-49 year-old immunosuppressed individual with additional chronic diseases reporting CRMNA was 20.3% (p< 0.001). Conversely, the predicted probability of a 75 year-old immunosuppressed individual without chronic diseases reporting CRMNA was as low as 2.5% (p< 0.001). Subgroup analysis among individuals with poor health (see Figure 2) showed that CRMNA was not associated with disease type (OR 0.63, 95% CI [0.33, 1.21], p=0.166 for immunosuppressed patients without chronic disease; OR 1.16, 95% CI [0.84, 1.60], p=0.353 for immunosuppressed patients with chronic disease).
Conclusion: These subgroup analyses show that rates of CRMNA among patients receiving immunosuppression differ widely across age groups, particularly among those with other chronic diseases. More than 15-20% of patients under the age of 49 years receiving immunosuppressives who had other chronic diseases reported CRMNA. This study highlights the need for a nuanced approach to evaluating and managing immunosuppressed patients at-risk for CRMNA.
To cite this abstract in AMA style:
Good S, England B, Volkmann E. High Rates of Cost-Related Medication Non-Adherence Among Younger Patients Receiving Immunosuppression Are Exacerbated by Other Chronic Conditions [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/high-rates-of-cost-related-medication-non-adherence-among-younger-patients-receiving-immunosuppression-are-exacerbated-by-other-chronic-conditions/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-rates-of-cost-related-medication-non-adherence-among-younger-patients-receiving-immunosuppression-are-exacerbated-by-other-chronic-conditions/