Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty occurs prematurely in RA. Levels of frailty are higher in Veteran populations than civilians1. Frailty has been shown to predict osteoporotic fractures in a single Canadian RA cohort, however the frailty instrument lacked external validation2. The aim of this study was to evaluate whether frailty predicted incident osteoporotic fractures in Veterans with RA using an externally validated frailty index.
Methods: We used data from the national Veterans Affairs Rheumatoid Arthritis (VARA) Registry 1/2003-12/31/2021. Baseline frailty was calculated using the VA Frailty Index (VAFI)1. The VAFI is based on diagnostic and CPT codes which are categorized into 31 deficits including morbidity, function, mood, cognition and geriatric syndromes. Osteoporotic fractures were identified by searching fracture-related diagnostic and procedure codes and subsequently validated by chart review. High-trauma, periprosthetic and pathologic fractures related to cancer were excluded. Missing data at baseline were imputed using multiple imputation with chained equations with 10 iterations and for further time points using the last observation carried forward. Age-adjusted fracture incidence rates were calculated. Multivariable Cox regression evaluating the relationship between baseline frailty and incident osteoporotic fracture was performed adjusting for baseline age, sex, race, smoking status, anti-cyclic citrullinated peptide (CCP) positivity and prior osteoporotic fracture; and time-varying body mass index (BMI), DAS28ESR, prednisone use, conventional synthetic disease modifying antirheumatic drug (DMARD) use, and biologic DMARD use. Participants were followed from enrollment and censored at osteoporotic fracture, death or end of study period.
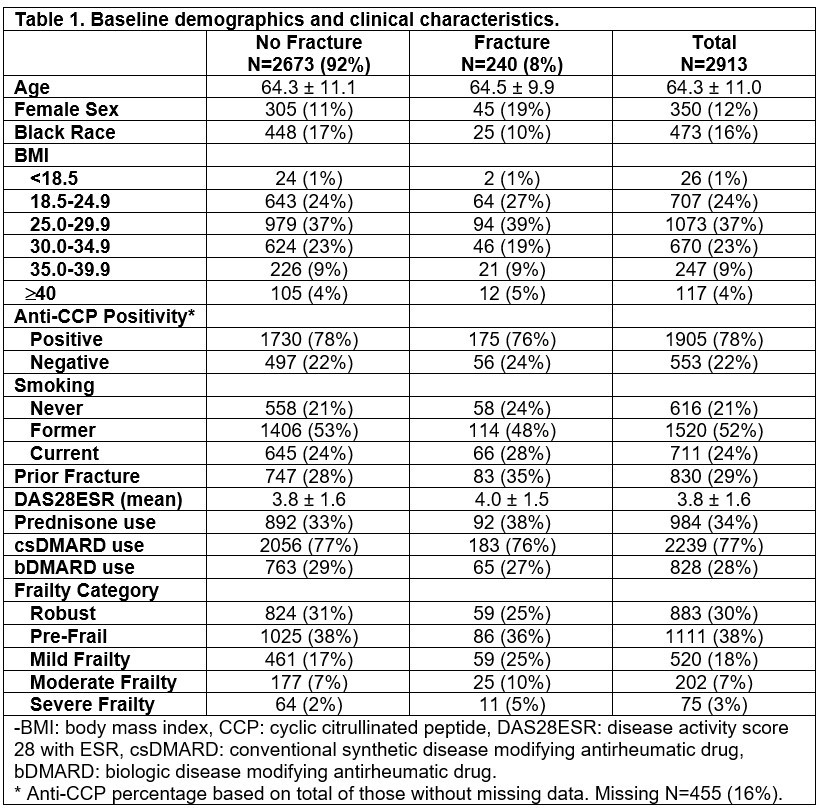
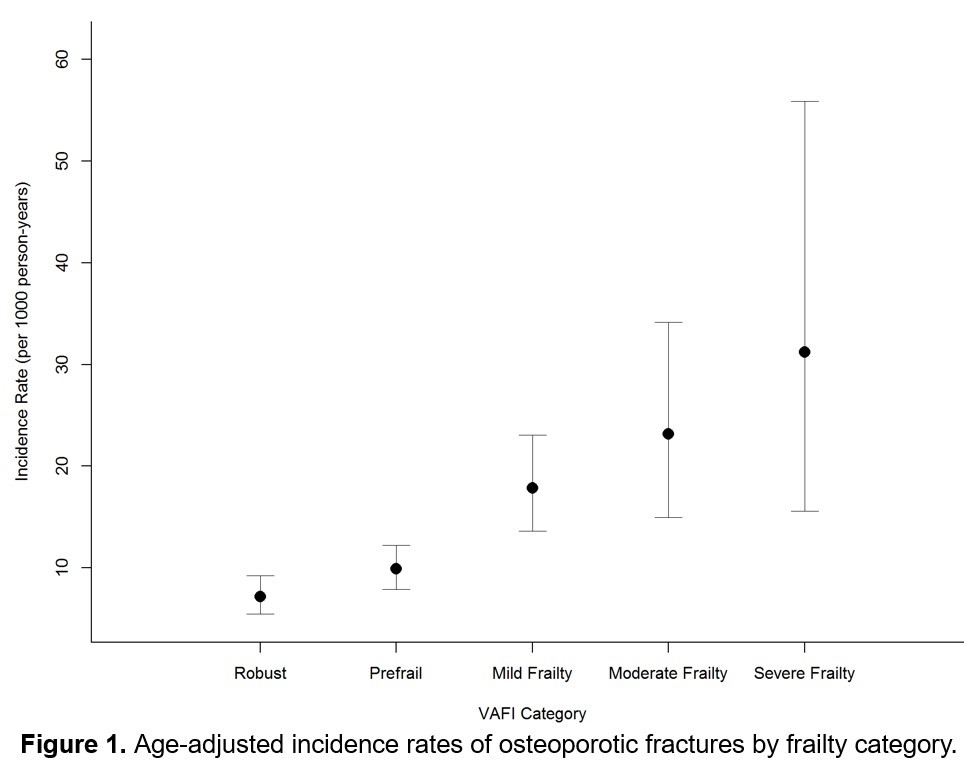
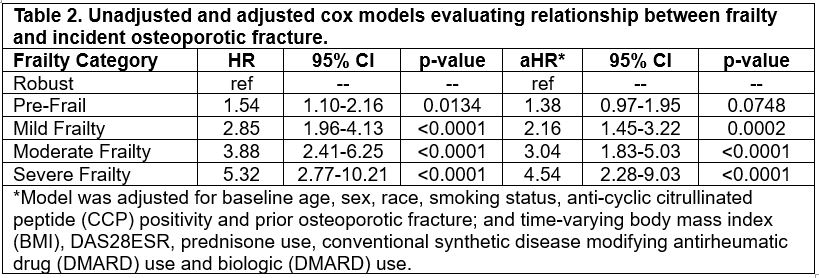
Results: 2,930 Veterans were included, mean age 64±11 years. Compared to those without incident osteoporotic fracture, those with fracture were more frequently female (19% vs 11%), less frequently Black (10% vs 17%) and had more pre-enrollment fractures (35% vs 28%) (Table 1). Age, anti-cyclic citrullinated peptide (CCP) positivity, BMI, disease activity and medication use at baseline were similar between those who did and did not fracture. There were higher rates of baseline frailty in the fracture group (25% vs 17% mild frailty, 10% vs 7% moderate frailty, and 5% vs 2% severe frailty). Over the 21,800 person-years of observation, 240 incident osteoporotic fractures occurred (79 extremity, 58 rib, 47 spine, 43 hip and 13 pelvis). Age-adjusted incidence rates of osteoporotic fractures increased by frailty category (Figure 1). In the multivariable Cox model, mild, moderate and severe frailty each had significantly increased risk of incident osteoporotic fracture compared to those who were robust (Table 2; aHR 2.16 [95% CI 1.45-3.22], 3.04 [95%CI 1.83-5.03] and 4.54 [95%CI 2.28-9.03]; all p< 0.001, respectively).
Conclusion: Baseline frailty is associated with incident osteoporotic fractures in Veterans with RA. Frailty measurement in RA using the VAFI, a validated, automated tool, may prove to be useful in identifying Veterans at high risk for osteoporosis and fractures. 1Orkaby AR et al. J Gerontol A Biol Sci Med Sci. 2019 2 Li G et al. Bone. 2019
To cite this abstract in AMA style:
Wysham K, Brubeck H, Baraff A, Roul P, Singh N, Andrews J, Cannon G, Kunkel G, Mikuls T, England B, Shoback D, Katz P, Garcia J, Orkaby A, Baker J. Frailty Is a Predictor of Incident Osteoporotic Fractures in Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/frailty-is-a-predictor-of-incident-osteoporotic-fractures-in-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-is-a-predictor-of-incident-osteoporotic-fractures-in-veterans-with-rheumatoid-arthritis/