Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Access to Janus kinase inhibitors (JAKi) is controlled by insurance carriers through prior authorizations and the use of restricted formularies. We previously showed that Black patients experienced an almost 2-fold longer delay in dispensing of JAKi compared to those who identified as Non-Hispanic White (Riley, ACR Convergence 2023). In this study, we hypothesized that key social factors were contributing to this observed disparity.
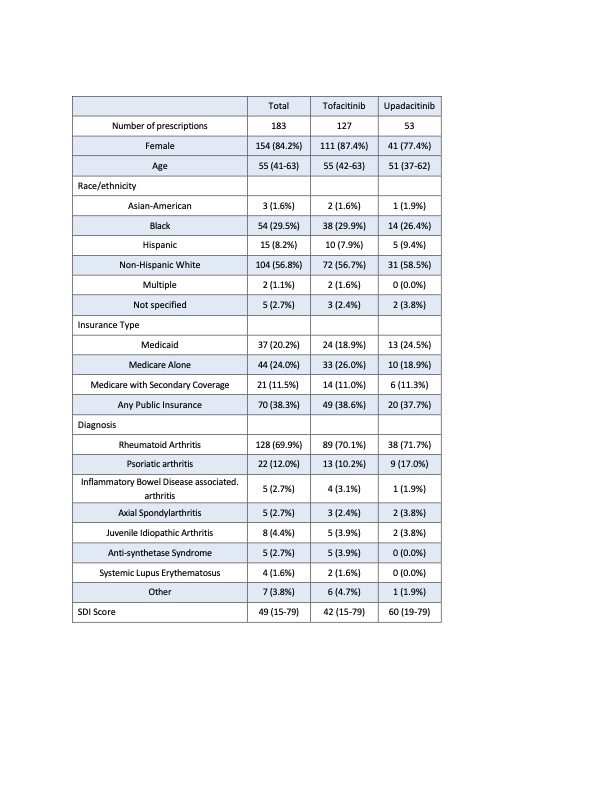
Methods: This retrospective cohort study included patients from an academic healthcare system with a documented JAKi prescription by a rheumatologist between 2014 and 2023, irrespective of underlying disease, allowing for multiple new JAKi prescriptions, but excluding existing prescription renewals. Demographics, details on insurance denials of coverage, and time to dispensation were extracted from the EHR, including pharmacy and nursing communications. ZIP-code tabulation area for each patient’s 5-digit ZIP-code was used to compute the Social Deprivation Index (SDI) score (range 0-100) for the year of the prescription. SDI is a measure of disadvantage based on seven demographic characteristics in the American Community Survey. Logistic and linear regression were used to determine if black race, SDI, public insurance, specialty pharmacy, or JAKi type were associated with denials of prescription or delays in dispensation, after adjustment for age, a diagnosis of rheumatoid arthritis vs. other condition, and prior use of a biologic therapy. A final model was developed that tested the effects of Black race on these outcomes with the addition of SDI, insurance status, specialty pharmacy, and JAKi type as confounders.
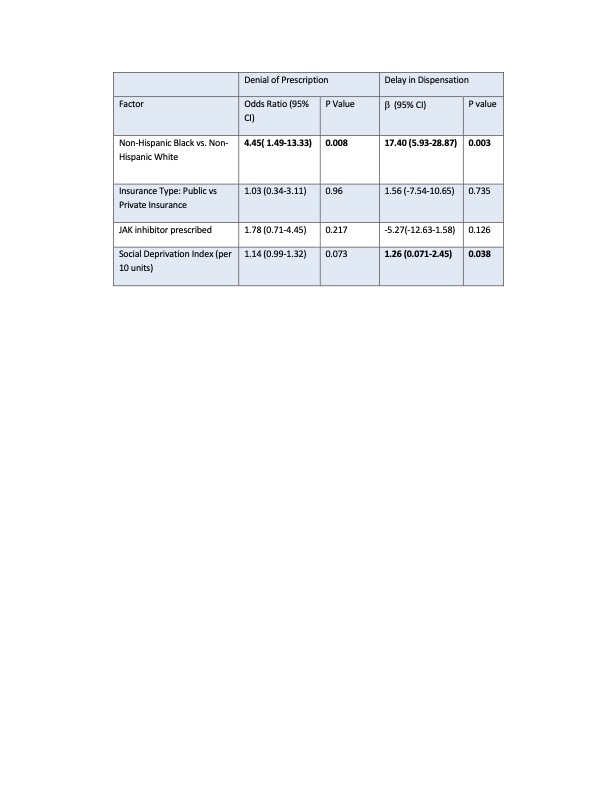
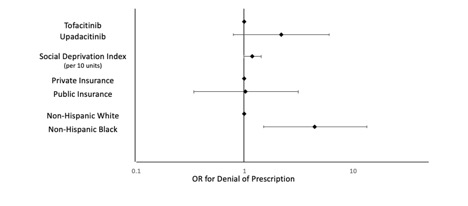
Results: 140 patients contributed 183 new JAKi prescriptions (Table 1). 18 prescriptions (9.8%) were denied by insurance, and the median time from prescription to dispensation was 13 days.In unadjusted regression analysis, patients who were Black had 4.45 higher odds of denial of prescription (OR 4.45, 95% CI 1.49-13.33, p=0.008), and if approved experienced a 17 day longer delay to dispensation (Β 17.40, 95 %CI 5.93-28.87, p =0.003) compared to patients who were White. A 10-point increase in SDI was not associated with denial but was associated with an additional 1.3-day delay in prescription dispensation (Β 1.26, 95% CI 0.071-2.45, p=0.038) (Table 2). JAKi type and other factors were not associated with denials or delays. These effects on denials and delays persisted in the adjusted model for those who were Black, but not for SDI. The addition of SDI, use of specialty pharmacy, public insurance status, and JAKi type did not explain the greater rates of denials or delays for patients who were Black (adjusted OR for denial 14.76 95% CI 2.27-96.17, p=0.005, Β for delays 21.71, 95% CI 8.59-34.82, p = 0.001).
Conclusion: Patients who were Black were more likely to experience denials and delays when prescribed JAKi. While SDI was associated with delays, this disparity for Black patients persisted despite adjustment for the SDI score and other factors, suggesting other barriers to equitable access not elucidated here. Further evaluation of the root of these disparities is needed, as well as work to understand the impact of delays in access to therapies on treatment outcomes.
To cite this abstract in AMA style:
Dombrovsky I, George M, Baker J, Riley T. Factors Associated with Delays in Dispensation and Insurance Denials of Janus Kinase Inhibitors [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/factors-associated-with-delays-in-dispensation-and-insurance-denials-of-janus-kinase-inhibitors/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-associated-with-delays-in-dispensation-and-insurance-denials-of-janus-kinase-inhibitors/