Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Seropositive RA is preceded by an at-risk stage characterized by elevated circulating autoantibodies (AAb), including ACPA, in otherwise healthy individuals without clinically-apparent inflammatory arthritis. Rising autoantibody levels prior to clinical diagnosis suggest changing immune activity but what additional immune dysregulation may be occurring in this period is incompletely understood. The purpose of this study was to profile the immune state that accompanies elevated AAb to identify novel immune features present in individuals at-risk (ARI) to develop clinical RA.
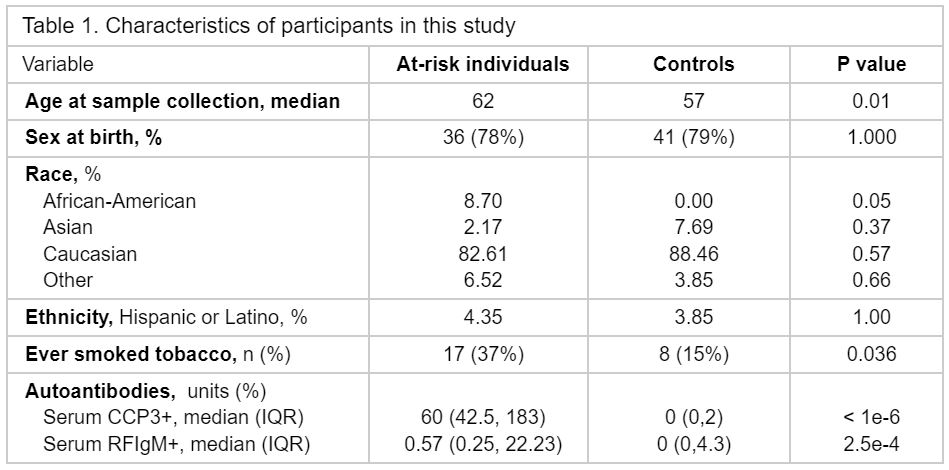
Methods: We profiled 1463 plasma proteins, 69 peripheral blood mononuclear cell (PBMC) phenotypes, and 1,973,362 PBMCs by single-cell RNA sequencing (scRNA-seq) for a cross-sectional analysis of ARI with high levels of ACPA (anti-CCP3 IgG > 40 units) compared to healthy control individuals (HCI) (Table 1). Linear regression models were used to identify differentially expressed proteins (ARI/HCI), and to identify lineage-defining gene programs in scRNA-seq. PBMC phenotypes were selected and analyzed based on their identification in the clinical RA literature to evaluate features of clinical disease present in ARI. Wilcoxon rank sum was used to evaluate the association of B cells to AAb levels. Finally, NicheNet was used to identify putative relationships between plasma proteins and gene expression in the target cells.
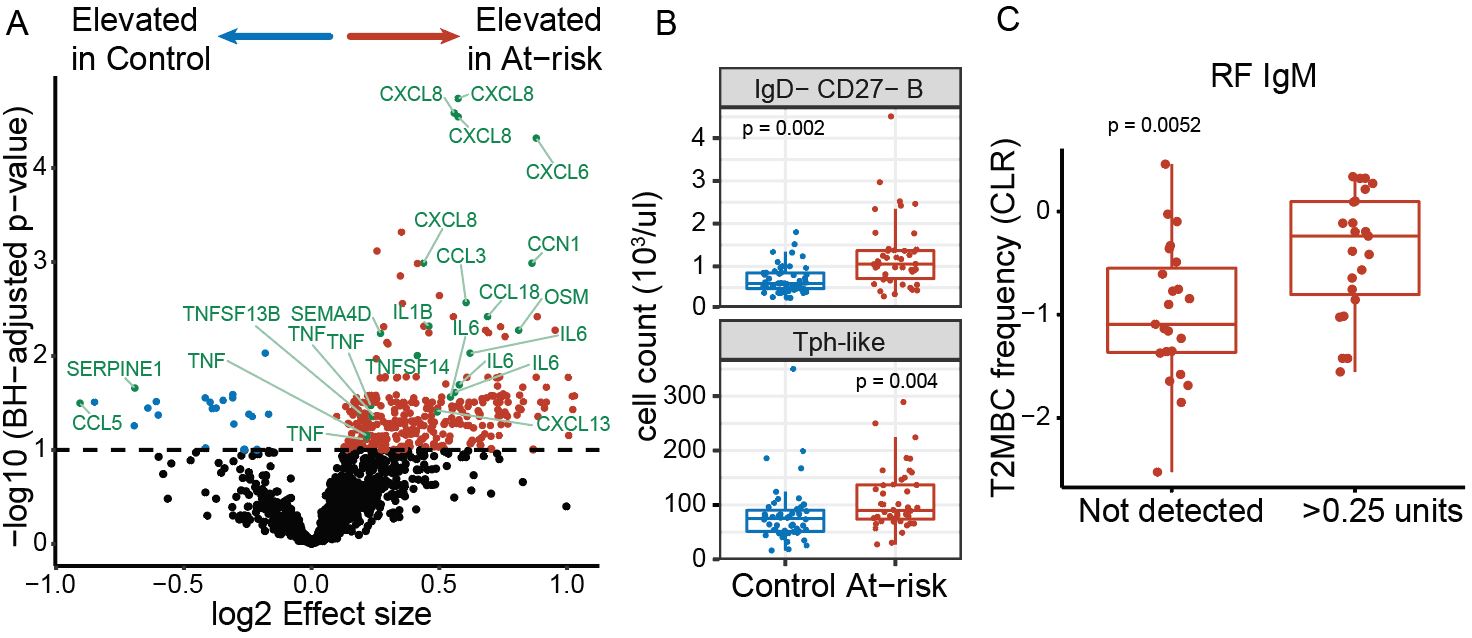
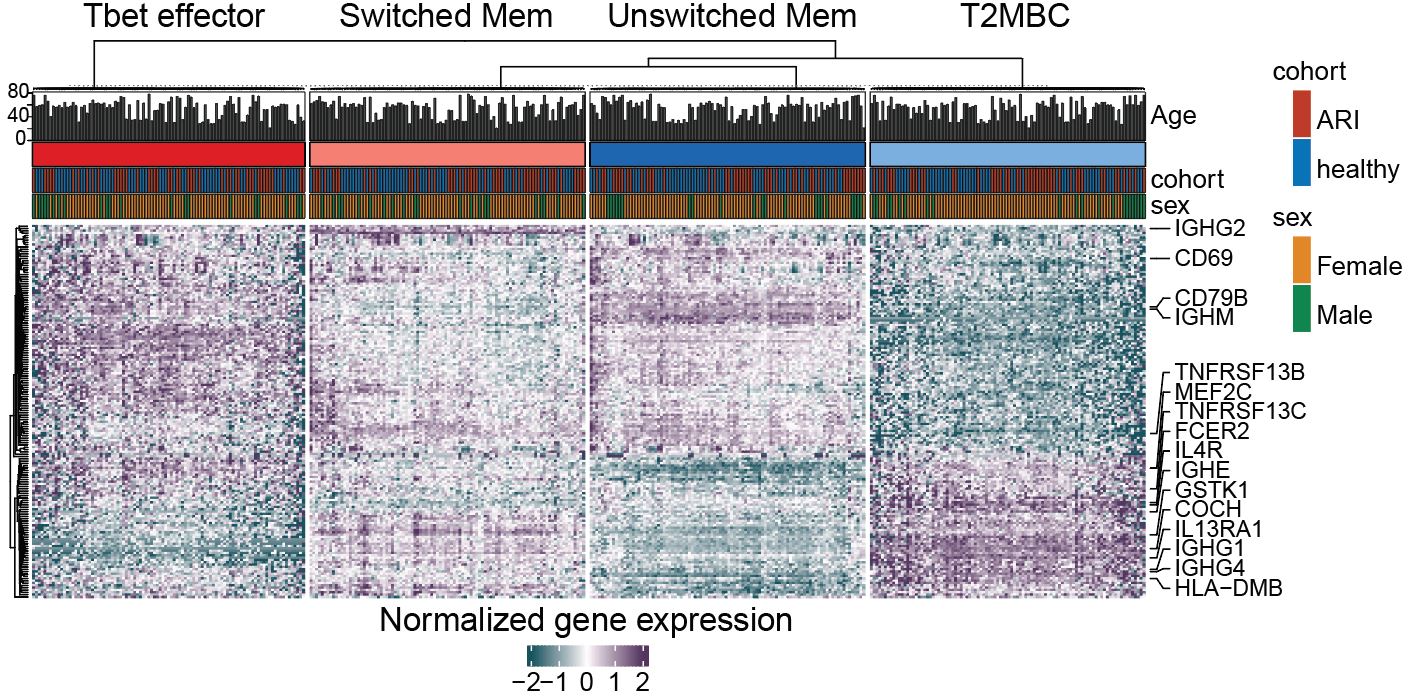
Results: 314 proteins exhibited significant differential expression between ARI and HCI, including CCN1, CXCL6, CCL18, OSM, CCL5, and SERPINE1, all of which were not previously reported in ARI, as well as proteins related to B cell biology, including CXCL13, SEMA4D, LIGHT, and BAFF (Fig 1A). In addition, we found evidence for features of classifiable RA, including increased IL-1B, IL-6, TNF, CCL3, and CXCL8 plasma proteins and elevated PBMC phenotypes. Among PBMC, atypical (IgD- CD27-) B cells and Tph-like (CXCR5- PD1+) CD4T cells (Fig 1B) were significantly increased. Transcriptomic analysis (scRNA-seq) of atypical B cells, enriched in ARI, demonstrated a gene program indicative of type 2-polarized memory B cells (T2MBC), including IL4R, IL13RA1, FCER2, IGHG4, IGHE, and MEF2C (Fig 2). T2MBC abundance was correlated to RF-IgM levels (Fig 1C). NicheNet analysis identified differentially-regulated proteins CCL3 (Pearson correlation coefficient (r) = 0.093), TNFSF13B (BAFF) (r = 0.077), TNFSF14 (LIGHT) (r = 0.048), and TNF (r = 0.047), as potential regulators of the T2MBC gene program.
Conclusion: We find that otherwise healthy at-risk individuals have immune dysregulation characterized by plasma protein and PBMC phenotype changes, including some that are similar to published findings in clinical RA. In particular, the number of T2MBC B cells were elevated in ARI and we recognized a relationship to RF-IgM AAb levels. Based on NicheNet analysis, we hypothesize that circulating plasma proteins in ARI reflect the maintenance or generation of T2MBC. These data deepen our understanding of this critical at-risk state and further emphasize the tight link between the dysregulation within the B cell compartment and autoimmune disease, which could be exploited for preventative therapeutic intervention.
To cite this abstract in AMA style:
Savage A, He Z, Glass M, Reading J, Moss L, Feser M, Tsaltskan V, Nguyen K, Demoruelle K, Kuhn k, Boyle D, Speake C, Li X, Skene P, Torgerson T, Bumol T, Holers V, Buckner J, Firestein G, Deane k, Gillespie M. Expansion of Atypical B Cells Accompanies Rheumatoid Arthritis-like Immune Dysregulation in ACPA+ At-risk Individuals [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/expansion-of-atypical-b-cells-accompanies-rheumatoid-arthritis-like-immune-dysregulation-in-acpa-at-risk-individuals/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/expansion-of-atypical-b-cells-accompanies-rheumatoid-arthritis-like-immune-dysregulation-in-acpa-at-risk-individuals/