Session Information
Date: Sunday, October 26, 2025
Title: (0671–0710) Systemic Sclerosis & Related Disorders – Clinical Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic sclerosis (SSc) is a connective tissue disease that can manifest as widespread skin and visceral fibrosis, potentially affecting major organs including the heart. Cardiac involvement is a major complication in SSc, often asymptomatic but associated with increased mortality. Despite recent improvement in survival and therapies, SSc remains the rheumatic disease associated with the highest morbidity and mortality. Cardiovascular magnetic resonance (CMR) is a sensitive, non-invasive tool for detecting cardiac abnormalities. However, the prognostic value of serial CMR monitoring and the effects of immunosuppressive therapy remain unclear. This study aimed to assess the prognostic significance of changes in CMR parameters for long-term cardiovascular outcomes, and to evaluate the impact of immunosuppressive treatments.
Methods: We conducted a monocentric retrospective study including consecutive SSc patients followed in the Internal Medicine department at Cochin University Hospital who underwent two CMR exams due to cardiovascular involvement. All patients met the American College of Rheumatology and European Alliance of Associations for Rheumatology 2013 classification criteria for SSc. Patients with two CMR scans performed on the same equipment between February 2009 and June 2023 were included, and parameter changes were compared using paired t-tests. The impact of treatments and CMR parameter changes on major adverse cardiovascular event (MACE) and all-cause mortality was assessed using Kaplan-Meier curves and log-rank tests.
Results: Forty-four SSc patients were included with a median [interquartile range] follow-up duration of 6.3 [3.1-9.2] years. The median interval between CMR scans was 1.5 [1.0-3.9] years. MACE occurred in 16 (33%) patients. There was no significant difference in the distribution of cardiovascular risk factors – including smoking (p=0.3), diabetes (p >0.9), and hypertension (p=0.7) – between patients who experienced MACE and patients who did not. In contrast, the prevalence of anti-Scl70 antibodies (p=0.023) and pulmonary hypertension (p=0.022) was higher among patients with MACE, although baseline functional, volumetric, and anatomical CMR parameters were not altered (Table 1). Right ventricle end-diastolic volume significantly decreased at the time of second CMR scan (p=0.04), contrary to maximal T1 (p=0.2), left ventricle end diastolic volume (p=0.1), left (p=0.5) and right (p=0.7) ventricular ejection fractions. Importantly, rituximab significantly decreased maximal T1 (p=0.029) (Figure 1), a marker of diffuse fibrosis also linked to an increased risk of all-cause death (p=0.044). Methotrexate was associated with a significant increase in left ventricular ejection fraction (p=0.032) (Figure 1) and a reduced risk of MACE (p=0.024).
Conclusion: Methotrexate use was associated with a decrease in MACE occurrence, highlighting a possible cardioprotective effect. Rituximab was linked to a decrease in maximal T1 value, a marker of diffuse fibrosis associated with increased mortality. These findings support the prognostic value of CMR monitoring and the potential benefit of immunosuppressive therapy in SSc-related cardiac involvement.
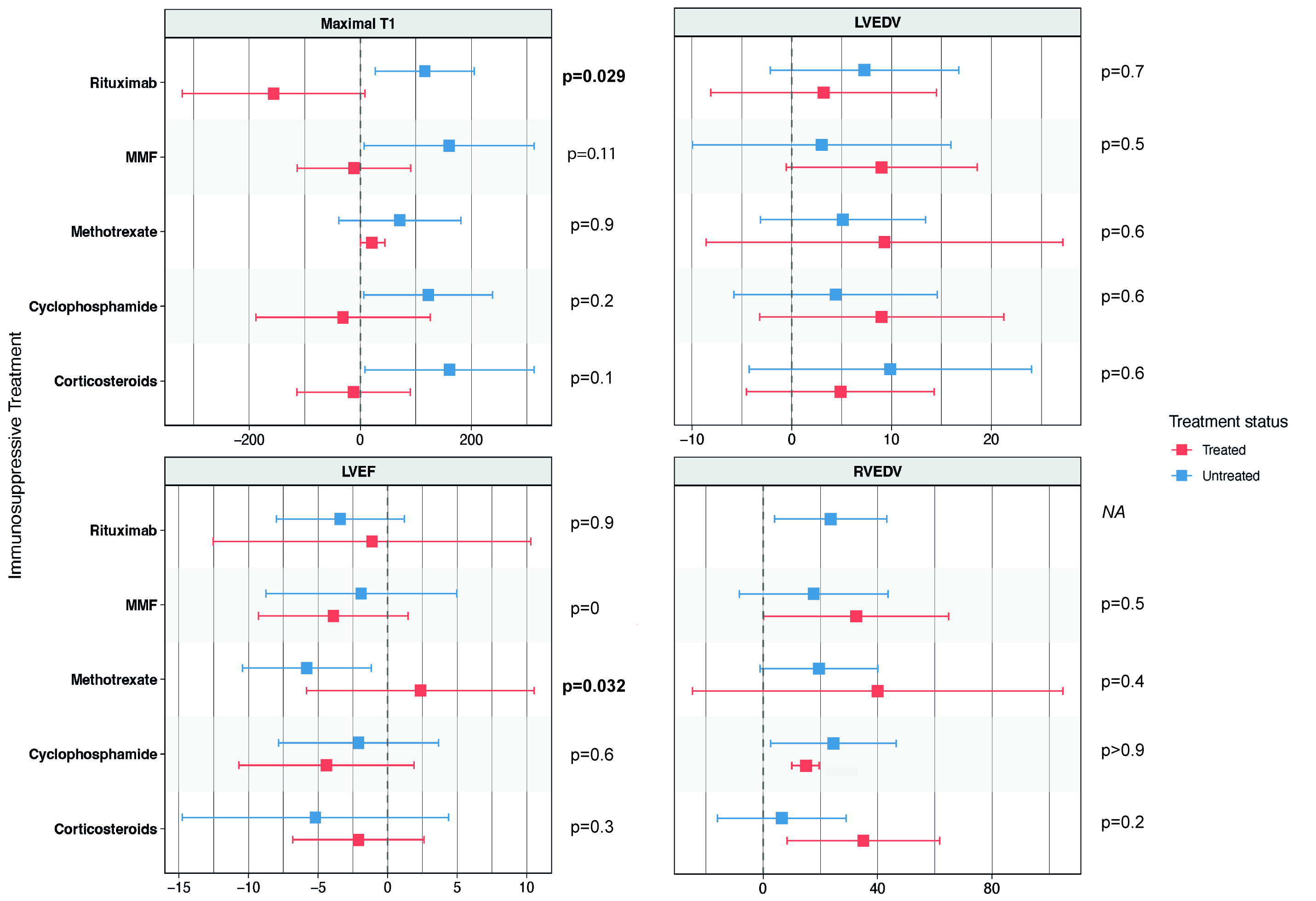 Table 1. Clinical, biological and CMR parameters data were collected at the date of first CMR examination (baseline), and stratified by MACE status. Continuous data are presented as median (Q1, Q3) and compared using a Wilcoxon rank sum exact test. Categorical variables are presented as n (%) and compared using Fisher’s exact test or Pearson’s Chi-squared test as appropriate.
Table 1. Clinical, biological and CMR parameters data were collected at the date of first CMR examination (baseline), and stratified by MACE status. Continuous data are presented as median (Q1, Q3) and compared using a Wilcoxon rank sum exact test. Categorical variables are presented as n (%) and compared using Fisher’s exact test or Pearson’s Chi-squared test as appropriate.
Abbreviations: ACE: angiotensin-converting enzyme; ANA: anti-nuclear antibodies; Anti-PM/Scl: anti-polymyositis/scleroderma antibodies; CMR: cardiovascular magnetic resonance imaging; LA: left atrium; LGE: late gadolinium enhancement; LV: left ventricle; LVEDV: left ventricle end diastolic volume; LVEF: left ventricle ejection fraction; MACE: major adverse cardiovascular events; mRSS: modified Rodnan skin score; PH: pulmonary hypertension; RV: right ventricle; RVEDV: right ventricle end-diastolic volume; RVEF: right ventricle ejection fraction; SSc: systemic sclerosis.
* Disease duration was determined from first non-Raynaud symptom.
† Obesity was defined by a body mass index ≥ 30 kg/m2.
‡ All PH were confirmed by right heart catheterization and defined by a mean Pulmonary Arterial Pressure > 20 mmHg.
.jpg) Figure 1. Forest plot representation of changes in CMR parameters stratified by immunosuppressive treatment.
Figure 1. Forest plot representation of changes in CMR parameters stratified by immunosuppressive treatment.
Mean differences in CMR measurements were compared between patients who received immunosuppressive therapies (including corticosteroids, mycophenolate mofetil, cyclophosphamide, rituximab, and methotrexate) and those who did not. Comparisons were performed using paired t-tests. Each square represents the mean difference, and the horizontal lines indicate the 95% confidence intervals. Patients treated with rituximab had a significant decrease in Maximal T1 value between 2 CMR scans.
Abbreviations: CMR: cardiac magnetic resonance imaging; LVEDV: left ventricle end diastolic volume; LVEF: left ventricle ejection fraction; RVEDV: right ventricle end-diastolic volume; RVEF: right ventricle ejection fraction.
To cite this abstract in AMA style:
Kante A, Mghaieth S, Dunogue b, berezne A, Comarmond C, Revel M, Chassagnon G, Mouthon L, Chaigne B. Evaluation of Serial Cardiovascular Magnetic Resonance Monitoring and Immunosuppressive Therapy in Predicting Long-Term Outcomes in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/evaluation-of-serial-cardiovascular-magnetic-resonance-monitoring-and-immunosuppressive-therapy-in-predicting-long-term-outcomes-in-systemic-sclerosis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/evaluation-of-serial-cardiovascular-magnetic-resonance-monitoring-and-immunosuppressive-therapy-in-predicting-long-term-outcomes-in-systemic-sclerosis/
